Key Highlights
- ADHD is highly genetic. Scientific evidence overwhelmingly shows that heritability plays the single largest role.
- ADHD is a biological, brain-based disorder, not the result of poor parenting, excessive sugar, or too many video games.
- Twin and family studies confirm ADHD runs in families. A child with a parent or sibling with ADHD is significantly more likely to have it.
- Specific genes, especially those involved with the neurotransmitter dopamine, are key risk factors.
- While genetics are the primary cause, environmental factors (like prenatal exposure to toxins) can contribute to or worsen symptoms.
- Current genetic testing cannot diagnose ADHD, but it can help personalize treatment by predicting medication response.
Introduction
Have you ever wondered what truly causes Attention-Deficit/Hyperactivity Disorder (ADHD)? It's a common question surrounded by myths. Many debate whether it's a product of genetics, environment, or lifestyle. The answer is clear: while we don't know every detail, medical research provides overwhelming evidence that ADHD is primarily a genetic condition.
This article will explore the science behind an ADHD diagnosis, separating fact from fiction to help you understand what causes this common neurodevelopmental disorder.
What is ADHD?
Attention-Deficit/Hyperactivity Disorder (ADHD) is a neurodevelopmental condition, not a character flaw or a failure of willpower. It is a brain-based, biological disorder with observable differences in brain structure, chemistry, and development.
Research from institutions like the National Institute of Mental Health shows that these brain differences are not caused by external factors like bad parenting, eating too much sugar, or excessive screen time. While those things might worsen symptoms, they don't cause the underlying condition.
In the United States, ADHD is a common condition affecting millions of children and adults. Understanding its biological basis is the first step toward dispelling myths and finding effective treatment.
What Are the Main Symptoms of ADHD?
ADHD symptoms are generally grouped into three presentations. A person may be diagnosed with one, based on which symptoms have been most prominent for the past six months.
- Predominantly Inattentive Presentation:
- Often overlooked or dismissed as "daydreaming."
- Difficulty sustaining attention in tasks or conversations.
- Prone to procrastination and disorganization.
- Loses things necessary for tasks (e.g., keys, wallet, phone).
- Forgetful in daily activities.
- Predominantly Hyperactive-Impulsive Presentation:
- Seems "driven by a motor"; feels restless (this can be internal in adults).
- Fidgets with hands or feet, or squirms in their seat.
- Talks excessively and may blurt out answers.
- Difficulty waiting their turn; often interrupts others.
- Combined Presentation:
- An individual meets the criteria for both inattentive and hyperactive-impulsive presentations.
These challenges often stem from difficulties with executive functioning of the brain's management system responsible for organization, time management, emotional regulation, and impulse control.
The Genetics of ADHD: What We Know So Far
The idea that ADHD is genetic is not a theory; it's a scientific consensus backed by decades of evidence.
Heritability Estimates from Family and Twin Studies
Twin studies provide the strongest proof of ADHD's genetic roots.
- Identical twins, who share 100% of their genes, have a very high concordance rate. If one identical twin has ADHD, the other is highly likely to have it as well.
- Fraternal twins, who share about 50% of their genes (like any other siblings), have a much lower concordance rate.
Family studies reinforce this. A child with ADHD is approximately four times more likely to have a relative with the condition. Research also shows that about one-third of fathers who had ADHD in their youth will have a child with ADHD.
Is It All Genetic? Genes vs. Environment
While genetics are the primary cause, environmental factors can play a secondary role. These factors do not cause ADHD on their own, but they may contribute to the risk or worsen symptoms, especially in someone already genetically predisposed.
Potential environmental risk factors include:
- Significant prenatal exposure to lead, BPA, or phthalates
- Premature birth or low birth weight
- Prenatal exposure to alcohol or nicotine
The overwhelming consensus, however, is that heritability accounts for the vast majority of ADHD cases.
Genes Linked to ADHD Risk
Scientists are now moving from "if" ADHD is genetic to "which genes" are involved.
Candidate Gene Studies and Their Findings
Candidate gene studies focus on specific genes suspected of being involved in a disorder. For ADHD, scientists have zeroed in on genes that manage brain chemistry.
The most prominent candidates are genes that control the neurotransmitter dopamine. Dopamine is crucial for regulating attention, motivation, and impulse control. Variations in genes that transport dopamine (like DAT1) are strongly linked to ADHD symptoms.
Genome-Wide Association Studies (GWAS) Insights
GWAS scans the entire genome of thousands of people to find genetic variants that are more common in those with ADHD. This "widenet" approach has confirmed that ADHD is a polygenic disorder.
This means ADHD is not caused by a single gene. Instead, it's caused by a combination of many possibly hundreds of common genetic variants, each contributing a small amount to a person's overall susceptibility.
Inheritance Patterns: Is ADHD Really Hereditary?
Yes. The high heritability means it is consistently passed down through generations. However, the way it's inherited is complex.
ADHD does not follow a simple "Mendelian" inheritance pattern (like eye color), where a single gene determines the outcome. It follows a complex inheritance pattern, where multiple genes and environmental factors interact. This explains why a parent with ADHD can have a child without it, or why the condition might seem to "skip" a generation.
Even when ADHD appears in multiple family members, the symptoms can look very different. One parent might have mild, inattentive ADHD, while their child has a severe, combined presentation. This is due to genetic diversity; each person inherits a unique combination of risk genes.
Can Genetic Testing Identify ADHD?
This is a critical question. Given the strong genetic link, can a DNA test diagnose ADHD?
No. Currently, there is no genetic test that can definitively diagnose ADHD.
The reason is its polygenic nature. Since hundreds of genes contribute, no single test can provide a "yes" or "no" answer. A person could have many "risk" genes and not have ADHD, while another could have fewer but still show clear symptoms.
Because of these limitations, an ADHD diagnosis is still based on a comprehensive clinical evaluation of symptoms, history, and impairment by a qualified mental health professional.
Personalizing ADHD Treatment with Pharmacogenetic (PGx) Testing
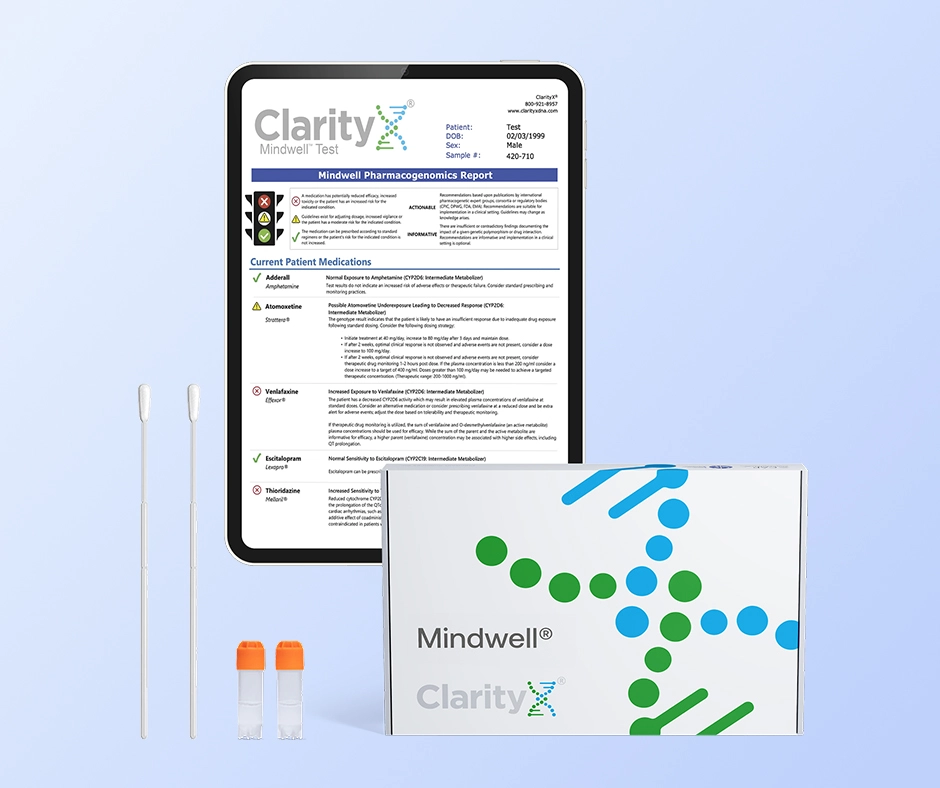
While genetic testing can't diagnose ADHD, it can play a crucial role in treating it. This is where pharmacogenetics (PGx) testing comes in.
Finding the right ADHD medication, particularly a stimulant, is often a frustrating "trial-and-error" process. A PGx test can help your doctor make a more informed decision from the start.
The ClarityX® Mindwell® test, for example, is a simple, at-home cheek swab. It analyzes your DNA to determine how your body is likely to process and respond to different medications. The test provides your doctor with a detailed report on:
- Metabolism: Whether you are a "poor," "normal," or "ultra-rapid" metabolizer for specific drugs, which can affect dosage.
- Efficacy: Which medications may be more likely to work for you.
- Side Effect Risk: Whether your genetics put you at a higher risk for adverse side effects from a particular medication.
This empowers your doctor to bypass some of the guesswork and personalize your treatment plan, leading to faster relief with fewer side effects.
Brain Changes and Neurobiology Related to Genetics
The genetic risk for ADHD translates into real, observable differences in the brain.
- Brain Structure: Imaging studies show that, on average, individuals with ADHD have slightly smaller (about 5%) brain volumes in key regions, particularly the prefrontal cortex (executive function), basal ganglia (impulse control), and cerebellum (coordination).
- Brain Development: Research also shows that these brain regions mature more slowly in children with ADHD.
- Brain Chemistry: As mentioned, the primary difference is in the dopamine system. ADHD is linked to lower levels of available dopamine, which disrupts communication between these critical brain regions, leading to symptoms of inattention and impulsivity.
The Role of Rare Genetic Variants and New Mutations
While most ADHD cases are polygenic (caused by many common genes), researchers are also studying the impact of rare genetic variants.
In some cases, a person may have a de novo mutation, a new genetic change that occurs spontaneously and is not inherited from either parent. These rare mutations can sometimes have a larger impact on brain development. This helps explain cases of ADHD where there is no known family history of the disorder.
Environmental Influences on ADHD
While genes are the primary driver, environmental factors can interact with a genetic predisposition.
- Prenatal Factors: Prenatal exposure to tobacco smoke, alcohol, or lead has been shown to increase the risk and severity of ADHD.
- Social and Cultural Factors: While a fast-paced, high-stimulation culture (social media, video games) does not cause ADHD, it can make symptoms more noticeable and problematic. The "epidemic of modernity" may exacerbate the challenges for a brain already wired for inattention.
Think of it this way: genes load the gun, but the environment can sometimes pull the trigger.
Myths About ADHD and Genetics
- MYTH: If a child has ADHD, a parent must have it.
- FACT: This is false. A child can inherit a specific combination of risk genes from both parents, even if neither parent has enough to be diagnosed. Also, a de novo mutation can be the cause.
- MYTH: If it's in my family, I'll definitely get it.
- FACT: This is genetic determinism, and it's incorrect. You inherit a risk or predisposition, not a guarantee. Protective environmental factors and interventions can make a huge difference.
- MYTH: If I don't have a family history, my ADHD must be caused by the environment.
- FACT: Not necessarily. Mental health conditions were often undiagnosed in previous generations, so the "family history" may simply be unknown. A new mutation could also be the cause.
Conclusion
Understanding that ADHD is a genetic, biological condition is the most important step in fighting stigma. It's not a choice, a moral failing, or a result of bad parenting. It's a difference in brain wiring and chemistry.
This genetic understanding has opened the door for new avenues of treatment. While genetics can't be used to diagnose ADHD, they can be used to personalize it. Tools like pharmacogenetic testing are moving treatment beyond a one-size-fits-all model and empowering individuals to find the right medication faster and with fewer side effects.
Frequently Asked Questions (FAQ)
Is ADHD more due to genes or environment in most cases? In most cases, ADHD is far more due to genes. Heritability for ADHD is estimated to be around 70-80%, which is among the highest for any psychiatric condition. This means genetics are the single largest contributing factor.
Can someone have ADHD if no one else in their family does? Yes. This can happen for several reasons: 1) The ADHD in previous generations was never diagnosed; 2) The person inherited a specific combination of "risk" genes from both parents that was just enough to express the condition; or 3) A new genetic mutation (a de novo mutation) occurred.
Are there ways to lower the "genetic risk" for ADHD? You cannot change your genetic predisposition. However, you can manage the symptoms and impairment. A healthy lifestyle (good sleep, regular exercise, balanced nutrition) can support brain health. More importantly, proven treatments like behavioral therapy, coaching, and proper medication can be life-changing.
Can you "grow out" of ADHD? You don't "grow out" of the genetic predisposition. However, the symptoms can change and often lessen with age. A hyperactive child may become a restless adult. Many adults develop highly effective coping strategies that allow them to manage their symptoms successfully, especially with the right treatment and support.
Resources:
https://www.psychiatry.org/patients-families/neurodevelopment-disorders
https://pmc.ncbi.nlm.nih.gov/articles/PMC6260148/
https://pubmed.ncbi.nlm.nih.gov/16123773/
https://medicover-genetics.com/genetic-disorders-monogenic-polygenic-and-chromosomal-disorders/
https://www.health.harvard.edu/mind-and-mood/dopamine-the-pathway-to-pleasure
https://my.clevelandclinic.org/health/body/prefrontal-cortex
https://clarityxdna.com/blog/learn/pharmacogenetic-testing-unlocking-personalized-medicine/