Key Highlights
Here are the main takeaways about the link between genetics and depression:
- Depression, also known as major depressive disorder, can run in families, suggesting a genetic link to this mental health condition.
- Genetics play a role, but they are not the sole cause; environmental factors and life events are also crucial.
- While researchers have identified several genetic variants, there is no single "depression gene" that causes the disorder.
- Having a close relative with depression may increase your risk, but it doesn't guarantee you will develop it.
- Genetic testing for depression exists, but its reliability for predicting risk is still under investigation.
Introduction
Have you ever wondered if depression is passed down through families? It's a common question for those affected by this mental illness. While the causes are complex, research shows that genetics do play a part in who develops a depressive disorder. This article explores the connection between your genes and your mental health, examining how family history, specific gene variants, and life experiences interact to influence your risk of experiencing depression symptoms. Understanding these factors is a key step in managing your well-being.
Understanding Depression: Defining the Condition
Depression, often called major depression or major depressive disorder, is a psychiatric disorder that impacts your mood, behavior, and overall health. It involves more than just feeling sad; it's characterized by prolonged feelings of hopelessness and a loss of interest in activities you once enjoyed.
It is one of the most common mental health conditions in the United States. To receive a diagnosis, a person must experience depression symptoms nearly every day for at least two weeks. While depression can be inherited, many people with the disorder have no family history of it.
Symptoms and Signs of Depression
Recognizing the symptoms of depression is the first step toward getting help. The signs can vary from person to person but often involve a combination of emotional and physical issues. The most common symptom is a persistent feeling of sadness or emptiness.
This emotional distress is frequently accompanied by a noticeable loss of interest in hobbies, work, or social activities you used to find pleasurable. You might also experience a significant loss of energy, feeling tired and fatigued most of the time. Other common symptoms and signs of depression include:
- Changes in appetite, leading to weight loss or gain
- Sleeping too much or having insomnia
- Difficulty concentrating or making decisions
- Unexplained aches, pains, or digestive problems
- Feelings of worthlessness or guilt
These symptoms can make it difficult to function in your daily life and can cause significant distress. If you recognize these signs, seeking professional support is essential.
Types of Depressive Disorders
"Depression" is an umbrella term for several related conditions. Understanding the different types can provide clarity on a specific diagnosis and guide treatment. The most well-known is major depressive disorder (MDD), which involves persistent symptoms that affect how you feel, think, and handle daily activities.
Other conditions are closely related. For example, some people experience depressive episodes as part of bipolar disorder, which also includes periods of mania. Another type is seasonal affective disorder (SAD), where symptoms appear and disappear with the changing seasons. These distinct disorders share features but have different triggers and patterns.
Here are a few common types of depressive disorders:
- Perinatal or Postpartum Depression: Occurs during pregnancy or after the birth of a child.
- Dysthymia (Persistent Depressive Disorder): A long-term form of depression with less severe but more chronic symptoms.
- Schizoaffective Disorder: A condition where depression occurs alongside symptoms of schizophrenia.
Impact on Daily Life
Depression's effects can extend into every corner of your life, making simple tasks feel overwhelming. Symptoms can make it difficult to function at school or work, leading to decreased performance and attendance issues. This can create a cycle of stress that worsens the condition.
Beyond work and school, depression significantly impacts relationships. The loss of interest and energy often leads to social isolation, as you may withdraw from friends and family. This lack of connection can deepen feelings of loneliness, complicating your mental health needs.
Physical health can also suffer. Depression is linked to other health conditions like chronic pain and digestive problems, and affected individuals have a higher risk of substance abuse issues. Addressing depression is crucial for your overall long-term health.
The Genetics Behind Depression
Depression is known to run in families, which strongly suggests that genetic factors contribute to the risk. If you have a family history of depression, you may have a genetic predisposition, meaning you could be more susceptible to the condition than someone without that same genetic makeup.
However, having a predisposition does not mean you will definitely become depressed. Research indicates that many different genetic variants, each with a small effect, likely combine to increase risk. It is this combination of genetic factors, rather than a single gene, that influences your vulnerability.
Inherited versus Genetic Depression: Key Differences
When discussing genetics, "hereditary" and "genetic" are often used interchangeably, but they have distinct meanings. A condition is genetic if it is influenced by your genes. In contrast, a hereditary condition is one passed down from a parent to a child through genes with a clear pattern of inheritance.
Depression is genetic because genetic factors play a role. However, it does not have a clear hereditary pattern like cystic fibrosis or Huntington's disease, because there isn't a single gene responsible.
Instead, a complex interplay of many genes and environmental factors determines your risk. This is why one person can have a family member with depression and never develop it, while another person with no affected close relatives can.
Family History and Its Influence
Having a family history of depression is one of the most significant risk factors. Studies show that individuals with a first-degree relative such as a parent or sibling with depression are about two to three times more likely to develop it themselves compared to the general population.
Your family history is just one piece of a much larger puzzle that includes your environment, lifestyle, and life experiences. Recognizing family history as a risk factor allows you to be more proactive about your mental health.
Key points to remember include:
- Genetics contribute to your overall risk.
- Environmental factors also play a critical role.
- A family history of depression doesn't seal your fate.
- Knowing your risk can empower you to seek support early.
Studies Supporting Genetic Links
Research into the genetics of depression has made significant strides. Large-scale studies involving thousands of individuals have been crucial in identifying potential genetic connections. These studies compare the DNA of people with depression to those without, searching for variations that appear more frequently in those with the disorder.
This research is still in its early stages but has provided valuable insights. Scientists believe many different genes, each contributing a small amount to the overall risk, are involved. This complexity is why pinpointing a single "depression gene" has been impossible. Future studies are needed to fully map out the genetic architecture of depression.
Specific Genes Associated with Depression
While the idea of a single "depression gene" is a misconception, researchers have identified several genes and genetic variants that may be associated with major depressive disorder. These genes have diverse functions in the brain, often related to how brain cells communicate or grow.
The current understanding is that variations in these genes can slightly increase your risk. It is the cumulative effect of multiple gene variants, combined with environmental factors, that contributes to the onset of depression.
Major Genes Identified in Research
Scientists are actively investigating various genes to understand their connection to depression. Instead of a single depression gene, a combination of genetic factors seems to play a significant role. The genes currently thought to be involved have a wide range of functions within the brain.
Some of these genes are responsible for managing neurotransmitters (chemical messengers like serotonin). Other genes under investigation are involved in the growth, maintenance, and adaptability of neurons.
Because so many gene variants might contribute to the risk in small ways, it is challenging to state definitively which ones are most important. It's likely that what we call depression may actually be multiple disorders with different underlying genetic contributors.
How Gene Variations May Impact Risk
Gene variations, or variants, are small changes in your DNA that make you unique. Think of eye color variants in certain genes determine whether your eyes are blue, brown, or green. Similarly, some genetic variants are associated with a higher or lower risk for developing conditions like depression.
Having a genetic variant linked to depression doesn't mean you will get it; it just means you may have a genetic predisposition. These variants can influence how your brain responds to stress or regulates mood, potentially making you more vulnerable to developing symptoms when faced with challenges.
It's the combination of multiple variants that shapes your risk:
- Some variants may affect brain chemistry and neurotransmitter levels.
- Others could influence how your brain adapts to experiences.
- The combined effect contributes to your overall genetic predisposition.
- These risk factors interact with your environment and lifestyle.
Emerging Genetic Discoveries
The field of genetics of depression is rapidly advancing. Thanks to large-scale, genome-wide association studies (GWAS), scientists are making progress. For instance, a 2018 study published in Nature Genetics identified 44 genetic variants associated with an increased risk for major depressive disorder.
This new research reinforces the idea that depression is a complex condition. Each identified variant contributes a very small amount to the overall risk, which explains why no single gene can be blamed. These discoveries are exciting because they offer new avenues for understanding the biological basis of depression. As our knowledge grows, these findings could one day lead to more personalized approaches to treatment.
Hereditability of Depression in Families
The question of how depression passes through families is a key area of mental health research. The fact that depression runs in families points to a heritable component. Studies involving twins and families have been instrumental in estimating how much of the risk is due to genetics versus environmental risk factors.
For example, studies on identical twins, who share 100% of their genes, offer powerful insights. If one twin has depression, the other is more likely to have it than a non-identical twin, suggesting a strong genetic link.
Twin and Family Study Insights
Twin and family studies are cornerstones of research into hereditary depression. By comparing rates of depression in identical twins versus fraternal twins (who share about 50% of their genes), scientists can estimate the heritability of the disorder.
When one identical twin has depression, the other twin has a significantly higher chance of developing it. This concordance rate is higher than for fraternal twins, indicating that shared genes are a major contributing factor.
However, since the concordance is not 100%, these studies also prove that genetics aren't the whole story. Environmental factors clearly play a crucial role in triggering depression, even in someone with a strong genetic predisposition.
What Is the Risk If Depression Runs in Your Family?
If you have a family history of depression, it is natural to worry. Research indicates that having a first-degree relative (a parent, sibling, or child) with depression gives you a two to three times higher risk of developing the condition.
This statistic highlights that genetics are an important risk factor, but it is far from a certainty. It's also crucial to know that many people who develop depression have no known family history of the disorder. This underscores that while family history is a known vulnerability, its absence doesn't grant immunity.
Patterns of Transmission Across Generations
Unlike single-gene disorders, depression does not follow a simple or predictable pattern of transmission. You can't use a simple chart to predict which family members will be affected. This is because multiple genes and environmental risk factors are involved.
A history of depression in your family is a clear risk factor. However, the disorder can appear to skip generations or affect relatives in different ways. For instance, one family member might experience a single depressive episode, while another might struggle with a chronic form.
- Depression does not have a clear pattern of inheritance.
- Having a first-degree relative with depression increases your risk.
- The severity and type of depression can vary among family members.
- Environmental triggers often interact with genetic vulnerability.
Epigenetic Factors Influencing Depression
Beyond your DNA sequence, there's another layer of genetic influence known as epigenetics. Epigenetic changes are modifications that can turn genes "on" or "off" without changing the DNA itself. These changes are often influenced by your environment, lifestyle, and experiences like trauma.
This means that even if you have a genetic predisposition, environmental factors can cause epigenetic changes that either increase or decrease your risk. This fascinating field helps explain how our experiences can "get under our skin" and affect our mental health.
What Are Epigenetic Changes?
Epigenetic changes are like switches on your genes. They don't alter your fundamental DNA code, but they do control which genes are active and which are silent. Think of your genes as a vast library of books; epigenetics determines which books are taken off the shelf and read.
These modifications can be triggered by a wide range of external factors, including your diet, exposure to toxins, and stress levels. Unlike the gene variants you are born with, some epigenetic changes can occur throughout your life. They represent a crucial link between your genes and your environment.
The Role of Stress and Trauma
Stress and trauma are powerful environmental stressors that can leave a lasting mark, partly through epigenetics. Experiencing stressful life events, such as childhood abuse or the loss of a loved one, can trigger epigenetic changes that activate a genetic vulnerability to depression.
This process helps explain why a person with a genetic predisposition might be fine for years, only to develop depression after a period of intense trauma. The external event acts as a switch, altering gene expression. Your genetic makeup might load the gun, but environmental factors like trauma can pull the trigger.
Behavioral and Environmental Epigenetics
Your behaviors and environment can directly influence your epigenetic landscape. Factors like diet, exercise, and sleep habits can cause changes that affect your mental well-being. Unhealthy behaviors like substance abuse are known environmental factors that can increase the risk of depression, partly by triggering adverse epigenetic modifications.
On the other hand, positive behaviors can act as protective factors. A healthy lifestyle, strong social connections, and effective stress management techniques may promote beneficial epigenetic changes. This highlights your agency in influencing your behavioral health. While you can't change your genes, you can modify your environment and behaviors.
Environmental Triggers of Depression
While genetics can create a predisposition, environmental factors often act as the trigger for a depressive episode. These triggers can include stressful life events, psychosocial stressors, and physical illnesses. Things like relationship difficulties, financial problems, or chronic pain can all contribute.
These environmental conditions can be powerful enough to cause depression even in individuals with no known genetic risk. Substance use is another major factor that can trigger or worsen depression.
Life Events That Can Cause Depression
Certain life events are potent causes of depression. These events are often characterized by loss, major change, or prolonged stress. The death of a loved one, a divorce, or the end of a significant relationship are common triggers.
Financial problems and unemployment can also create a chronic sense of hopelessness. Similarly, experiencing social isolation or ongoing relationship difficulties can leave you feeling alone and unsupported.
While anyone can be affected by these events, they can be especially challenging for individuals who may already be vulnerable. Some common life events that can cause depression include:
- The death of a loved one
- Divorce or relationship breakdown
- Job loss or financial instability
- Childhood abuse or neglect
- Chronic illness or pain
- Major life transitions
Interaction Between Genetic and Environmental Influences
Depression rarely stems from a single cause. Instead, it is most often the result of a complex interaction between genetic factors and environmental factors. Think of it as a dialogue between your nature (your genes) and your nurture (your experiences).
Your genetic makeup can create a certain level of vulnerability. However, this vulnerability may never lead to depression unless it is activated by external risk factors, such as stress or trauma. This gene-environment interaction is central to understanding who develops depression and why.
Can You Develop Depression Without Genetic Risk?
Yes, you can absolutely develop depression even if you have no known genetic risk or family history. While genetics can increase susceptibility, powerful environmental stressors and life events can be sufficient to trigger depression on their own.
Many people who experience depression do not have any affected relatives. Their condition can often be traced back to factors like severe stress, trauma, or a major physical illness. These experiences can profoundly impact brain chemistry, leading to the symptoms of depression. This is an important reminder that depression can affect anyone.
Genetic Testing for Depression Risk
Many wonder about genetic testing for depression risk. While some tests claim to provide insights into genetic depression risk, the science is still in its early stages. According to government organizations like the National Institutes of Health, there is currently no single test that can definitively tell you if you will develop depression.
The complexity of depression makes creating a reliable predictive test very challenging. Before making any decisions based on genetic testing, it's crucial to understand their limitations.
Genetic Testing For Depression Medication
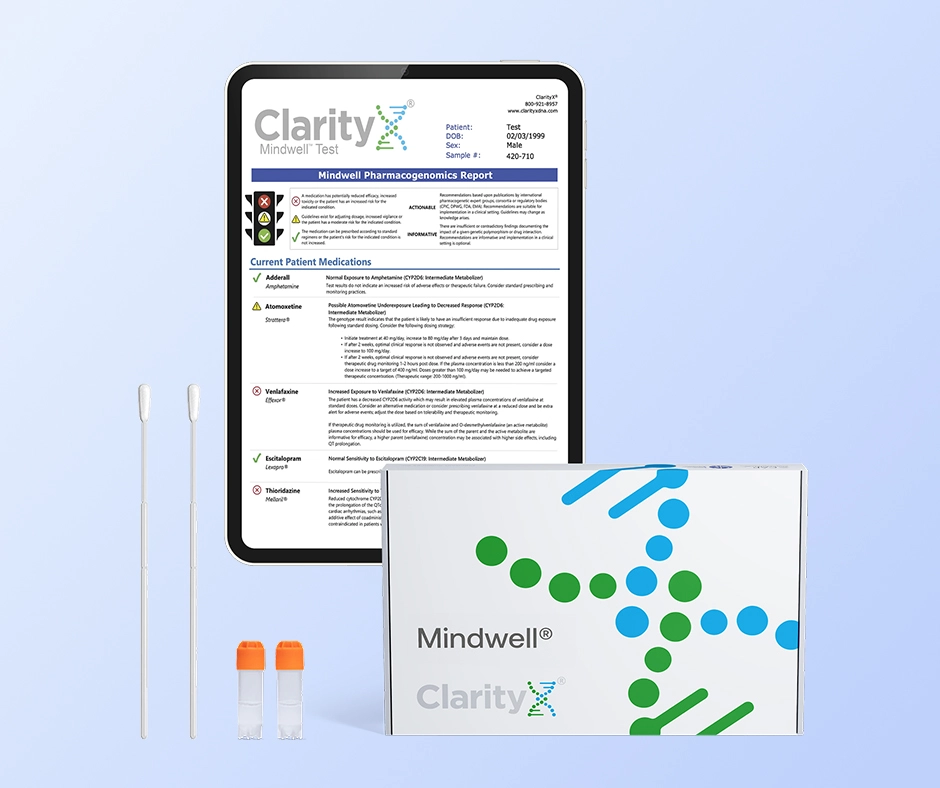
It is important to distinguish predictive testing (for risk) from a different, actionable type of genetic test: pharmacogenetic (PGx) testing.
While a genetic test can't reliably predict if you will develop depression, a PGx test can help predict how you may respond to medications once you have been diagnosed.
This field is called pharmacogenetics. A simple, non-invasive ClarityX® Mindwell® test ( just a cheek swab) analyzes how your specific genes influence your body's response to certain drugs. For depression, this is incredibly valuable as it can provide insights on:
- Metabolism: How quickly or slowly your body breaks down specific antidepressants (like SSRIs).
- Side Effect Risk: Whether your genes put you at a higher risk of experiencing side effects from a particular medication.
- Efficacy: Which medications are more likely to be effective for you based on your unique genetic profile.
This information helps your doctor move beyond a "trial-and-error" approach, allowing them to make a more informed, personalized choice for your treatment plan from the start.
Conclusion
In summary, understanding the genetic components of depression is crucial. While genetics can play a significant role in determining susceptibility, it is equally important to consider the influence of environmental factors and life experiences. The interplay between genetic predisposition and external triggers creates a complex landscape that shapes mental health outcomes. By staying informed about the latest research, you can better navigate your own mental health journey.
Frequently Asked Questions
How do I know if my depression is genetic or caused by my environment? It's nearly impossible to separate the two, as depression is usually caused by an interaction between genetic factors and environmental factors. A strong family history suggests a genetic link, but stressful life events often trigger the onset of symptoms. Ultimately, your mental health is a product of both nature and nurture.
Is postpartum depression genetic? Yes, like other forms of major depression, postpartum depression (PPD) is believed to have a strong genetic component. If you have a close family member with depression or PPD, your risk may be higher. However, it's a complex interplay of genetic vulnerability, the dramatic hormonal changes after childbirth, and environmental stressors like lack of sleep and social support.
Can epigenetic changes be reversed? Some epigenetic changes may be long-lasting, but others are potentially reversible. Lifestyle modifications like exercise, a healthy diet, and stress management can act as protective factors that may influence your epigenome positively. This is an active area of research.
Is anxiety inherited in the same way as depression? Anxiety and depression are different mental disorders, but they share similar inheritance patterns. Both often run in families and involve a complex mix of multiple genetic factors and environmental triggers. Like mood disorders, anxiety is not caused by a single gene, and a family history indicates an increased risk, not a certainty.
Resources:
https://www.ncbi.nlm.nih.gov/books/NBK559078/
https://www.nimh.nih.gov/health/publications/seasonal-affective-disorder
https://clarityxdna.com/blog/bipolar-disorder-medication-what-are-your-options/
https://clarityxdna.com/blog/postpartum-depression-what-every-new-parent-should-know/
https://www.science.org/content/blog-post/there-no-depression-gene
https://www.verywellmind.com/what-is-a-neurotransmitter-2795394
https://www.nature.com/articles/s41588-018-0090-3
https://www.cdc.gov/genomics-and-health/epigenetics/index.html