Key Highlights
- Depression has a genetic component, with research suggesting that around 40% of people with the condition can link it back to genetic factors.
- Having a family history of depression, such as a parent or sibling with the condition, increases the risk of developing depression.
- Environmental factors, such as childhood trauma or severe life stress, can also contribute to the development of depression.
- Treatment options for depression include antidepressant medications and therapy, such as cognitive behavioral therapy.
- Prevention strategies for depression involve early detection, intervention, and support for at-risk individuals.
- Lifestyle changes, such as maintaining a healthy diet, regular exercise, and managing stress, can help reduce the risk of depression.
Introduction
Depression is a common mental health disorder that affects millions of people worldwide. It is characterized by persistent feelings of sadness, emptiness, and a loss of interest in activities. While the exact cause of depression is not fully understood, research suggests that there is a genetic component to the condition. In other words, some individuals may have a higher risk of developing depression due to their genetic makeup.
Having a family history of depression can increase the likelihood of developing the condition. Studies have shown that individuals with a first-degree relative, such as a parent or sibling, with depression may have a two to four times greater risk of experiencing depression themselves. This suggests that genetic factors play a role in the development of depression.
However, it's important to note that genetics is not the sole determinant of depression. Environmental factors, such as traumatic life events, chronic stress, and certain medical conditions, can also contribute to the onset of depression. Understanding the interplay between genetics and environmental factors is crucial in order to effectively prevent, diagnose, and treat depression.
In this blog, we will explore the genetic and environmental factors that contribute to depression, the role of genetics in the development of the condition, treatment options, and prevention strategies. By understanding the underlying causes of depression, we can better support individuals who are at risk and provide effective interventions to improve mental health outcomes.
Understanding Depression
Depression, also known as major depressive disorder, is a common mental health condition that affects a person's mood, thoughts, and overall well-being. It is characterized by persistent feelings of sadness, hopelessness, and a loss of interest or pleasure in activities.
Depression is a serious condition that can significantly impact a person's daily functioning and quality of life. It is classified as a mood disorder, along with other conditions such as bipolar disorder. While everyone experiences feelings of sadness or grief at times, depression is different in that it involves prolonged periods of intense sadness and a lack of enjoyment in life. This can lead to social withdrawal and can impact important responsibilities like work or school.
Depression is a complex condition with various factors that contribute to its development. It can be caused by a combination of genetic, environmental, and psychological factors. Understanding the different aspects of depression is crucial in order to provide effective treatment and support for individuals experiencing this condition.
Defining Depression: More Than Just Sadness
Depression, or major depressive disorder, is a mental illness that goes beyond temporary feelings of sadness. It is characterized by persistent and intense feelings of sadness, hopelessness, and a lack of interest or pleasure in activities that were once enjoyable.
The symptoms of depression can vary from person to person, but common signs include changes in appetite and sleep patterns, low energy levels, difficulty concentrating, feelings of guilt or worthlessness, and can include thoughts of death or suicide. These symptoms often interfere with daily activities and can significantly impact a person's quality of life.
Depression is a serious mental illness that requires professional treatment and support. It is not a sign of weakness or a character flaw but rather a medical condition that can be effectively managed with the right interventions. If you or someone you know is experiencing symptoms of depression, it is important to seek help from a mental health professional.
Symptoms and Diagnosis: Recognizing Depression in Yourself and Others
Recognizing the symptoms of depression is essential for early diagnosis and intervention. While everyone experiences sadness or low moods at times, it is important to differentiate between temporary feelings and the persistent symptoms of depression.
Common depressive symptoms include a persistent sad or irritable mood, loss of interest or pleasure in activities, changes in appetite or weight, sleep disturbances, fatigue or loss of energy, feelings of worthlessness or guilt, difficulty concentrating, and recurring thoughts of death or suicide.
A diagnosis of depression is typically made by a mental health professional, such as a psychiatrist or psychologist. They will evaluate the presence and severity of symptoms, as well as the duration of symptoms, in order to determine if it meets the criteria for major depressive disorder.
It is important to remember that depression is a treatable condition, and seeking professional help is crucial for effective management. If you or someone you know is experiencing symptoms of depression, it is important to reach out to a healthcare professional for support and guidance.
The Genetics of Depression
The role of genetics in the development of depression has been the focus of extensive research. While it is clear that there is a genetic component to the condition, the exact genes and mechanisms involved are still being explored.
Studies have shown that individuals with a family history of depression, such as a parent or sibling with the condition, have a higher risk of developing depression themselves. This suggests that there are specific gene variants that may contribute to the development of the condition.
However, it is important to note that genetics is not the sole determinant of depression. Environmental factors, such as stressful life events and other social and psychological factors, can also play a significant role in the development of the condition. The interplay between genetics and the environment is complex and requires further study to fully understand its impact on depression.
What Research Says About Depression and Genetics
Twin studies have provided valuable insights into the genetic link to depression. These studies involve comparing the rates of depression between identical twins, who share 100% of their genes, and fraternal twins, who share approximately 50% of their genes.
Research has consistently shown that there is a higher concordance rate for depression in identical twins compared to fraternal twins. This suggests that genetic factors play a significant role in the risk of developing depression.
However, it is important to note that genetics is not the sole determinant of depression. Environmental factors, such as stressful life events, can also contribute to the development of the condition, even in individuals with a genetic predisposition.
How Genes Influence Depression: A Closer Look
Genes play a crucial role in the development of depression, but it is important to understand that there is no single "depression gene." Instead, depression is influenced by multiple genetic factors.
Research suggests that different genes are involved in the development of depression, each with a small effect. These genes contribute to the overall genetic component of depression.
It is also important to note that genes do not act in isolation. They interact with environmental factors to influence the risk of developing depression. This complex gene-environment interaction requires further study to fully understand its impact on the development of the condition.
Environmental Factors and Depression
While genetics play a significant role in the development of depression, environmental factors also contribute to the risk of developing the condition. Stressful life events, such as the loss of a loved one, relationship problems, financial difficulties, or exposure to trauma, can trigger or exacerbate depressive symptoms.
Environmental factors can interact with genetic factors to increase the risk of developing depression. For example, individuals with a genetic predisposition to depression may be more vulnerable to the effects of stressful life events.
Understanding the interplay between genetics and the environment is crucial in order to effectively prevent and treat depression. By addressing both genetic and environmental factors, healthcare professionals can provide a comprehensive approach to the management of depression.
Life Events and Stress: How They Trigger Depression
Traumatic events and chronic stress can have a significant impact on mental health, including the development of depression. Exposure to traumatic events, such as physical or sexual abuse, accidents, or natural disasters, can trigger the onset of depressive symptoms.
Chronic stress, such as ongoing financial difficulties, work-related stress, or relationship problems, can also contribute to the development of depression. Prolonged exposure to stress can disrupt the body's stress response systems and increase the risk of developing both mental and physical health conditions. With increased stress comes increased cortisol levels. When cortisol remains elevated long-term, the effects can be far-reaching, including higher rates of heart disease, more susceptibility to infection, and an increased risk of mental health disorders like depression.
These environmental factors can interact with genetic factors to increase the risk of depression. Individuals with a genetic predisposition to depression may be more vulnerable to the effects of traumatic events or chronic stress.
Understanding the role of environmental factors in the development of depression is essential in order to effectively prevent and treat the condition. Stressors are not always avoidable, so it is crucial to identify and learn to manage them effectively. By addressing both genetic and environmental factors, healthcare professionals can provide comprehensive care for individuals with depression.
Interplay Between Genetics and Environment
While genetic factors play a significant role in predisposing individuals to depression, the environment also contributes considerably to its development. The interplay between genetics and environmental influences is complex.
Stressful life events, childhood trauma, and socio-economic factors can interact with genetic predispositions to increase the risk of depression. Understanding how these factors interact can provide valuable insights into personalized treatment approaches that consider both genetic susceptibilities and environmental triggers. This intricate relationship highlights the importance of a holistic approach to addressing depression.
Depression Across the Lifespan
Depression can affect individuals of all ages, from children to older adults. The symptoms and manifestations of depression can vary depending on the age group.
Childhood and adolescent depression may present with symptoms such as irritability, social withdrawal, changes in appetite or sleep, academic difficulties, physical complaints, or thoughts of suicide. It is important to recognize the early signs of depression in children and provide appropriate support and intervention.
Adults and elderly individuals may experience symptoms such as persistent sadness, a loss of interest in activities, changes in appetite or sleep, fatigue, difficulty concentrating, or thoughts of death or suicide.
Understanding the unique aspects of depression across the lifespan is crucial in order to provide targeted interventions and support for individuals of all ages.
Childhood and Adolescent Depression: Early Signs
Recognizing the early signs of depression in children and adolescents is essential for early intervention and support. Some common early signs of childhood depression include persistent sadness, irritability, social withdrawal, changes in appetite or sleep patterns, academic difficulties, or physical complaints such as headaches or stomach aches.
It is important to note that these symptoms can be indicative of other issues as well, and a thorough evaluation by a mental health professional is necessary for an accurate diagnosis. Early intervention is crucial for preventing the long-term consequences of childhood depression.
Childhood depression can have a significant impact on brain development and overall well-being. By identifying and addressing depressive symptoms early on, healthcare professionals can provide appropriate support and intervention to promote healthy development and well-being in children and adolescents.
Depression in Adults and the Elderly: Differences in Manifestation
Depression in adults and the elderly may present with similar symptoms to childhood and adolescent depression, but there are also some unique aspects to consider.
In adults, symptoms of depression can include persistent sadness, a loss of interest in activities, changes in appetite or sleep, feelings of guilt or worthlessness, fatigue, difficulty concentrating, or recurring thoughts of death or suicide.
Elderly individuals may experience similar symptoms, but depression in older adults can often be masked by other physical health conditions or attributed to normal aging. It is important to recognize the signs of depression in the elderly and provide appropriate support and intervention.
Understanding the differences in the manifestation of depression across different age groups is crucial in order to provide targeted interventions and support for individuals of all ages.
Treatment Options for Depression
Depression is a treatable condition, and there are various treatment options available. The most common treatments for depression include medication and therapy.
Antidepressant medications can help relieve the symptoms of depression by balancing the levels of chemicals in the brain that are associated with mood regulation. There are different types of antidepressant medications available, such as selective serotonin reuptake inhibitors (SSRIs), serotonin-norepinephrine reuptake inhibitors (SNRIs), and tricyclic antidepressants (TCAs). SSRIs like escitalopram, fluoxetine, and others have become some of the most commonly prescribed medications for depression early in therapy. Working with a healthcare professional is important to find the right medication and dosage for your individual needs.
Therapy, such as cognitive behavioral therapy (CBT), can also be an effective treatment for depression. CBT focuses on identifying and changing negative thought patterns and behaviors that contribute to depressive symptoms. Other forms of therapy, such as interpersonal therapy (IPT) and psychodynamic therapy, may also be helpful in addressing underlying issues and promoting emotional well-being.
Combining medication and therapy often provides the best outcomes for individuals with depression. Working with a healthcare professional to develop a personalized treatment plan that addresses your specific needs and goals is important.
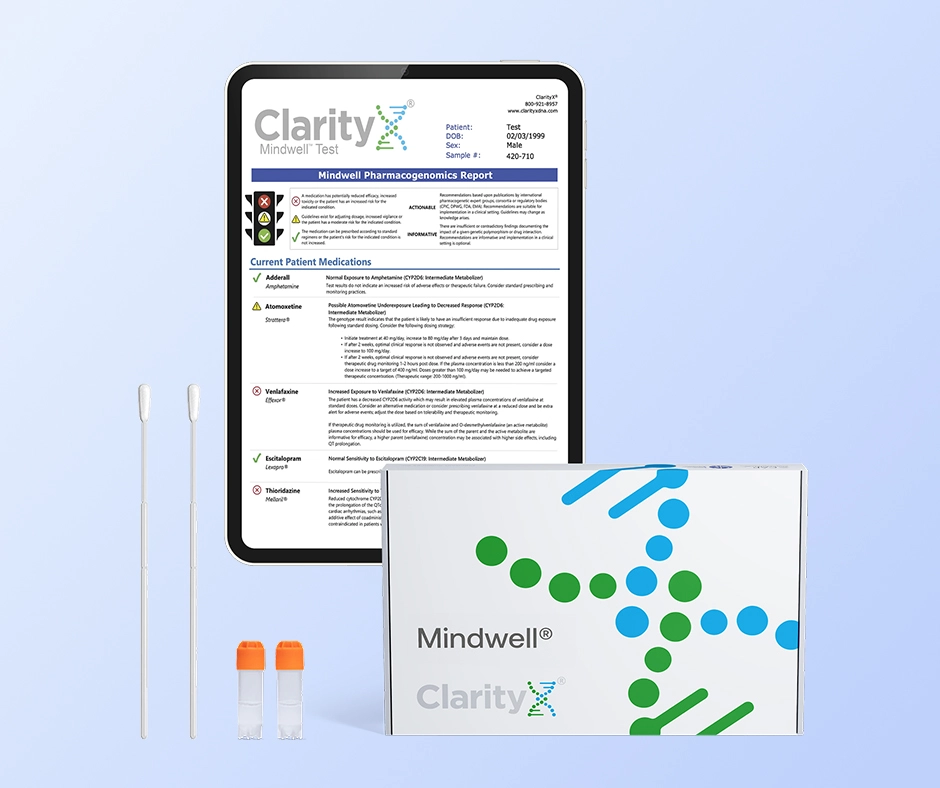
Medication and Genetics: Finding the Right Match
Genetic factors can significantly impact how effective antidepressant medications can be and how likely they are to cause side effects. Tailoring medication to the individual's genetic makeup can optimize outcomes. Based on genetic testing, personalized medicine helps identify which medications are most suitable for a patient. Understanding how genes influence the body's response to antidepressants is key to finding the right match. By considering genetic factors, healthcare providers can navigate the complex landscape of depression treatment more effectively. Matching medication to genetics holds promise for improving patient care and outcomes.
Therapy and Lifestyle Changes: Non-Genetic Interventions
In addition to medication, therapy, and other treatments, lifestyle changes can also play a significant role in the management of depression. While genetics may contribute to the risk of developing depression, lifestyle factors can influence its severity and course.
Cognitive behavioral therapy (CBT) is a type of therapy that focuses on identifying and changing negative thought patterns and behaviors that contribute to depressive symptoms. It can help individuals develop healthier coping mechanisms and improve their overall well-being.
Lifestyle changes, such as maintaining a healthy diet, regular exercise, getting enough sleep, managing stress, and engaging in pleasurable activities, can also support mental health and reduce symptoms of depression. These non-genetic interventions can provide additional support and improve overall well-being.
Working with a healthcare professional to develop a comprehensive treatment plan that addresses genetic and non-genetic factors is important. By combining medication, therapy, and lifestyle changes, individuals can effectively manage their depression and improve their quality of life.
Preventing Depression
While it may not be possible to completely prevent depression, there are strategies that can help reduce the risk and promote mental well-being. Prevention strategies focus on early detection, intervention, and support for individuals who are at risk.
Identifying at-risk individuals, such as those with a family history of depression or individuals who have experienced traumatic events, is an important step in prevention. Providing support and resources to these individuals can help them manage stress and build resilience.
Early detection and intervention are crucial in preventing the onset and progression of depression. Healthcare professionals, family, and friends can all play a key role in identifying symptoms and providing appropriate support and treatment.
Prevention strategies also involve promoting mental health and well-being through education, awareness campaigns, and providing resources and support. By addressing risk factors and promoting mental well-being, we can reduce the impact of depression on individuals and communities.
Strategies for At-Risk Individuals
For individuals at risk of depression due to genetic factors or family history, early interventions and lifestyle adjustments can be pivotal. Regular exercise, proper nutrition, adequate sleep, and stress management techniques can help mitigate the likelihood of developing major depression. For help with stress management, meeting with a therapist to help define sources of stress and personalized strategies to better manage life’s stressors can be very helpful.
Engaging in supportive social activities, seeking therapy, and building resilience through mindfulness practices are also beneficial strategies. Monitoring symptoms closely and seeking professional help when needed are crucial steps in the prevention of depression in at-risk populations.
Importance of Early Detection and Intervention
Early detection and intervention are crucial in effectively managing depression and reducing its impact. Recognizing the signs and symptoms of depression early on can lead to prompt intervention and improved outcomes.
Healthcare professionals play a key role in early detection. By conducting thorough assessments and evaluations, they can identify symptoms of depression and provide appropriate support and treatment. Family, friends, and community members can also help by fostering a non-judgmental, supportive environment.
Early intervention involves providing the necessary resources and interventions to individuals experiencing depressive symptoms. This may include therapy, medication, lifestyle changes, and other supportive measures. The goal is to address symptoms early on and prevent the escalation of the condition.
Access to mental health services is essential in supporting early detection and intervention. By providing accessible and affordable mental health services, individuals can receive the support they need at the earliest stages of depression.
By prioritizing early detection and intervention, healthcare professionals can provide timely and effective support for individuals with depression, leading to improved outcomes and better overall mental health.
Conclusion
In conclusion, understanding the interplay between genetics and environmental factors is crucial in comprehending the complexities of depression. While genetic predispositions may play a role, environmental triggers can also significantly impact its onset and severity. Recognizing the symptoms, seeking appropriate treatment, and creating a supportive environment are key steps in managing depression effectively. Remember, you are not alone; seeking help and addressing concerns is a sign of strength, not weakness. If you have concerns about depression, reach out to mental health professionals for guidance and support. Your well-being matters.
When considering treatment options your genetics can also play a vital role in determining which medications will be best suited for you. A simple test can help reduce the trial and error process associated with finding the right medication. Find out more by visiting www.clarityxdna.com
Frequently Asked Questions
Can Depression Be Completely Cured?
Depression is a treatable condition, but it may not be completely cured for everyone. The goal of treatment is to manage symptoms and improve quality of life. The duration of treatment may vary depending on the individual and the type and severity of depression.
How Can I Tell If My Depression Is Genetic?
Identifying if your depression is genetic involves looking at your family history. If you have a first-degree relative, such as a parent or sibling, with depression, you may have a higher risk of developing the condition. Genetic testing can also provide more information about your individual genetic risk factors.
What Are the Chances of Inheriting Depression?
The chances of inheriting depression can vary depending on various factors. Research suggests that individuals with a family history of depression are more likely to develop the condition. Studies with twins have shown that there is a higher concordance rate for depression in identical twins compared to fraternal twins, indicating a genetic predisposition.
Can Lifestyle Changes Override Genetic Predisposition to Depression?
While genetic predisposition can increase the risk of developing depression, lifestyle changes can play a significant role in managing the condition. Engaging in regular exercise, maintaining a healthy diet, managing stress, and seeking support can help reduce the impact of genetic predisposition and promote mental well-being.
Where to Find Support and Resources
Finding support and resources is crucial for individuals with depression and their loved ones. Support groups, mental health resources, and healthcare professionals can provide valuable guidance and assistance. Various organizations and online platforms offer support and information for individuals with depression and their families.
Resources
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3077049/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6065213/
https://www.ncbi.nlm.nih.gov/books/NBK559078/
https://www.apa.org/ptsd-guideline/patients-and-families/cognitive-behavioral
https://www.ncbi.nlm.nih.gov/books/NBK554406/
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3897684/
https://my.clevelandclinic.org/health/diseases/14938-depression-in-children