Key Highlights
- Adult ADHD and major depressive disorder frequently co-occur, presenting challenges in accurate diagnosis and effective treatment.
- ADHD symptoms like poor concentration and impulsivity can overlap with depressive symptoms, making it hard to distinguish between these mental health issues.
- The risk of developing depression increases significantly for those with untreated or undiagnosed ADHD.
- Proper assessment and early intervention are essential to manage comorbid disorders and improve daily life.
- Evidence-based treatments, including a combination of medication and behavioral therapy, offer the best outcomes for those affected.
- Understanding unique risk factors, such as family history and substance misuse, helps guide targeted interventions.
Introduction
Understanding attention deficit hyperactivity disorder (ADHD) and depression is crucial for anyone concerned about mental health. Both are psychiatric disorders with unique and overlapping features, often leading to confusion in diagnosis. Depression symptoms, such as persistent sadness and loss of interest, can, at times, look similar to ADHD traits like inattention and low motivation. Recognizing the distinct and shared indicators of these mental disorders helps you or your loved ones seek the right support and treatment for better well-being.
Defining ADHD and Depression
ADHD is classified as a neurodevelopmental disorder, marked by attention deficits, impulsivity, and hyperactivity. These ADHD symptoms frequently appear in childhood but can persist as adult ADHD, affecting daily life and relationships. The diagnosis of ADHD requires a clinical assessment focusing on behavioral patterns over time.
In contrast, depression is a mood disorder that includes major depression and other depressive disorders. A depressive episode often features ongoing sadness, hopelessness, and loss of interest. While both are mental disorders, distinguishing between their presentations is essential for accurate diagnosis and timely support.
What are the key differences in symptoms between ADHD and depression, and how can they be accurately distinguished from each other? While ADHD is tied to attention, hyperactivity, and impulsive actions, depression is centered around low mood, energy loss, and negative self-perception. Understanding the duration, triggers, and context of these symptoms is key to telling them apart.
Clinical Features of ADHD
ADHD is primarily characterized by symptoms such as inattention, impulsivity, and hyperactivity. People, especially those with childhood ADHD, may struggle with maintaining focus, organizing tasks, and completing projects. In adult ADHD, these challenges often continue, manifesting as disorganization, forgetfulness, and difficulty meeting daily responsibilities.
The nervous system plays a crucial role since ADHD is rooted in neurodevelopment. Poor concentration is common, but unlike depression, it’s usually present throughout a person’s life and not triggered by mood episodes. Hyperactivity disorder signs might appear as restlessness or fidgeting, which can persist into adulthood, though sometimes in subtler forms, such as mental restlessness rather than physical.
What are the key differences in symptoms between ADHD and depression, and how can they be accurately distinguished from each other? Unlike depression, ADHD’s core features revolve around long-standing attention deficits and hyperactivity, while mood fluctuations are typically short-lived. Major depressive episodes, on the other hand, include persistent sadness and loss of interest lasting weeks or months.
Clinical Features of Depression
Depression, especially major depressive disorder or severe depression, is mostly defined by persistent depressive symptoms. These include feeling sad, hopeless, or empty, and sometimes manifest as irritability. Core signs of depression are loss of interest in previously enjoyed activities, fatigue, and changes in sleep or appetite.
Many people with depressive disorder find it difficult to concentrate or make decisions, but unlike ADHD, these issues start with or worsen during depressive episodes. Behavioral withdrawal, such as avoiding social interactions or neglecting self-care, is also common. Severe depression can lead to suicidal thoughts or feelings of worthlessness, which require immediate professional attention.
What are the key differences in symptoms between ADHD and depression, and how can they be accurately distinguished from each other? While both conditions can show poor concentration, depression’s cognitive difficulties are episodic and linked to low mood. ADHD’s attention issues, in contrast, are present from a young age and are not driven by emotional states.
Distinguishing Symptoms: ADHD vs Depression
Differentiating between ADHD symptoms and symptoms of depression can be tough since both impact concentration and motivation. However, the underlying causes and duration of these mental disorders provide important clues. Diagnosis of ADHD centers on lifelong patterns of inattention and impulsivity, while depression is defined by changes in mood, energy, and pleasure lasting at least two weeks.
Accurate diagnosis relies on identifying whether poor focus is a constant challenge (ADHD) or a new problem linked to low mood (depression), ensuring the right intervention.
Emotional and Behavioral Differences
Emotional and behavioral patterns help set ADHD and depression apart. Symptoms of ADHD often include impulsive decisions, quick emotional responses, and difficulty maintaining attention. These behaviors usually reflect a lifelong pattern and respond well to behavioral therapy.
Mood disorders like depression, however, are marked by a persistent low mood, an inability to feel pleasure, and social withdrawal. Whereas people with ADHD may be seen as “always on the go,” those experiencing depression often feel slowed down or stuck.
Poor concentration is a common thread, but in ADHD, it's linked to distraction and restlessness, while in depression, it's rooted in lack of motivation and overwhelming sadness. Recognizing if the main struggle is attention deficit or emotional downturn is key to distinguishing between the two and selecting the right treatment approach.
Overlapping Symptoms and Challenges in Diagnosis
Overlapping symptoms are a significant challenge in the diagnosis of ADHD and depression. Both may present with poor concentration, fatigue, and restlessness, raising the risk of misdiagnosis, especially in young people and adult patients.
Common overlapping symptoms include:
- Difficulty concentrating
- Irritability or restlessness
- Changes in sleep patterns
- Low motivation or energy
These shared features can confuse clinicians, but careful assessment of onset, duration, and associated mood changes can clarify the diagnosis. Clinicians are advised to gather information from multiple sources, such as self-reports and family observations, to avoid confusing ADHD symptoms for depressive symptoms or vice versa. Recognizing these overlapping areas helps ensure accurate mental health treatment and reduces the likelihood of inappropriate or ineffective interventions.
Prevalence and Co-occurrence in the United States
In the United States, the prevalence of ADHD and depressive disorders is notable, particularly among adult patients. Rates of comorbid disorders are higher than once thought, with many individuals experiencing both an ADHD diagnosis and major depressive disorder. This co-occurrence complicates both identification and treatment.
Understanding patterns of prevalence and comorbidity is essential for health professionals, as it highlights the need for thorough screening and comprehensive care plans to manage both conditions effectively in daily life.
How Often Do ADHD and Depression Occur Together?
Comorbid ADHD and depression are more common than many realize. Research shows that between 19% and 53% of people with ADHD also experience a depressive disorder. Adult ADHD significantly raises the risk of developing depressive symptoms, and vice versa.
Here’s a summary table highlighting the prevalence:
The likelihood of having both conditions increases with certain risk factors, such as gender, inattentive ADHD subtype, and family history of mental disorders. Awareness of these trends can prompt early assessment and targeted intervention.
Risk Factors for Dual Diagnosis
Several risk factors make having both ADHD and depression more likely. Genetics, environmental influences, and personal history all play a part.
Major risk factors include:
- Family history of ADHD, depression, or other psychiatric disorders
- Substance misuse or presence of substance use disorders
- Comorbid anxiety disorders or other mood disorders
- Early-onset ADHD or untreated ADHD in young people
Stressful life events, such as trauma or chronic stress, can also increase susceptibility. Recognizing these risk factors allows for proactive screening and intervention, especially in individuals already diagnosed with one mental health condition. Early identification can greatly improve outcomes and help break the cycle of worsening symptoms.
The Link Between Untreated ADHD and Depression
The connection between untreated ADHD and the development of depression is well documented in mental health research. Adults and young people with undiagnosed or untreated ADHD face a heightened risk of developing depressive symptoms over time. Struggles with self-esteem, social difficulties, and academic or work setbacks can contribute to the progression from attention deficit symptoms to major depression.
Untreated ADHD not only increases the risk for depression but can also worsen its severity, making timely diagnosis and intervention critical for long-term well-being.
How ADHD May Lead to Depression
Living with undiagnosed or untreated ADHD can be challenging, resulting in emotional difficulties that raise the risk of depression. Chronic feelings of failure, repeated setbacks in school or work, and negative feedback from others can erode self-esteem and resilience. For many, this constant struggle leads to major depression or persistent depressive disorder.
The risk of depression is even higher when ADHD-related problems, such as academic underachievement, relationship issues, or impulsivity, begin early in life. Research shows that people with ADHD are more likely to experience depressive episodes, especially when their symptoms remain unmanaged.
Comorbid disorders, such as anxiety or substance misuse, can further complicate this relationship. Addressing ADHD symptoms early and comprehensively can lower the likelihood of developing serious mood disorders later in life.
Impact of Comorbid ADHD and Depression on Daily Life
When ADHD symptoms and depression symptoms occur together, the impact on daily life is often profound. People with both conditions tend to experience more severe impairments than those with just one condition.
Key effects include:
- Reduced ability to manage work or school tasks due to attention deficits and low motivation
- Difficulty maintaining relationships because of mood swings and impulsivity
- Increased risk of substance misuse and poorer overall mental health
- Lowered quality of life, with higher rates of social withdrawal, low self-worth, and even suicidal thoughts
Adults with comorbid ADHD and depression may also face challenges in daily organization and self-care. Support from mental health professionals, family, and community resources becomes even more critical to help navigate these complex challenges.
Assessment and Misdiagnosis Considerations
Correctly identifying ADHD and depression is crucial, given that overlapping symptoms can easily lead to misdiagnosis. Many major depressive disorder and psychiatric disorders share similar traits with ADHD, which can result in inappropriate treatment if not carefully evaluated. Misdiagnosis can delay effective ADHD treatment or support for depressive disorder.
A detailed assessment, involving clinical interviews, rating scales, and information from multiple sources, helps avoid these pitfalls. Recognizing the nuances in symptom presentation ensures that individuals receive tailored, effective care.
Screening Tools for ADHD and Depression
To increase accuracy in diagnosis, the American Psychiatric Association recommends using validated screening tools for both ADHD and depression. These tools support clinicians in distinguishing between overlapping symptoms and determining the most pressing mental health needs.
Common screening and diagnostic tools include:
- The Adult ADHD Self-Report Scale (ASRS) for adult ADHD symptoms
- The Patient Health Questionnaire (PHQ-9) for depressive symptoms
- Mood and Feelings Questionnaire (MFQ) for children and adolescents
- Structured clinical interviews for both disorders
Behavioral therapy assessments also provide insight into functional impairments. Using a combination of these tools, clinicians can gather comprehensive data, reduce the risk of misdiagnosis, and design more effective, individualized treatment plans for those with complex presentations.
Red Flags That Help Differentiate Conditions
Certain signs can alert clinicians and individuals to the presence of either ADHD symptoms or signs of depression, aiding in a more accurate diagnosis of ADHD or major depressive disorder.
Key red flags include:
- ADHD symptoms: Lifelong attention difficulties, impulsivity, and hyperactivity, with onset in childhood
- Signs of depression: Sudden changes in mood, energy, or appetite, persistent sadness or hopelessness
- ADHD-related poor concentration is consistent and unaffected by mood, while depression-related attention issues worsen with emotional distress
- Major depressive disorder is marked by loss of pleasure, while ADHD is characterized by disorganization and distractibility without pervasive sadness
Clinicians should also watch for a family history of psychiatric disorders and significant shifts in functioning. Identifying these red flags improves assessment accuracy and ensures interventions target the core problem.
Evidence-Based Treatments for Co-occurring ADHD and Depression
Treating co-occurring ADHD and depression requires a tailored approach, often including a combination of medication and behavioral therapy. ADHD treatment may include stimulants or nonstimulant medications, while depressive episodes are managed with antidepressants or specific therapies.
A comprehensive treatment plan addresses both disorders, taking into account the most impairing symptoms and personal preferences. Collaboration between clinicians, patients, and families is vital to ensure safe, effective management of these complex, comorbid disorders.
Medication Strategies and Considerations
Medication options for comorbid ADHD and depression must be chosen with care. ADHD medications, such as stimulants (e.g., Adderall), can improve focus but sometimes have side effects like sleep disturbances or appetite suppression, which may mimic or worsen depressive symptoms.
When symptoms of depression are predominant, antidepressants like bupropion (Wellbutrin) may be prescribed, it can address both depressive disorder and some ADHD symptoms. Treating one condition can sometimes ease the other; studies reveal that ADHD medication may lower the risk of depression by as much as 20%.
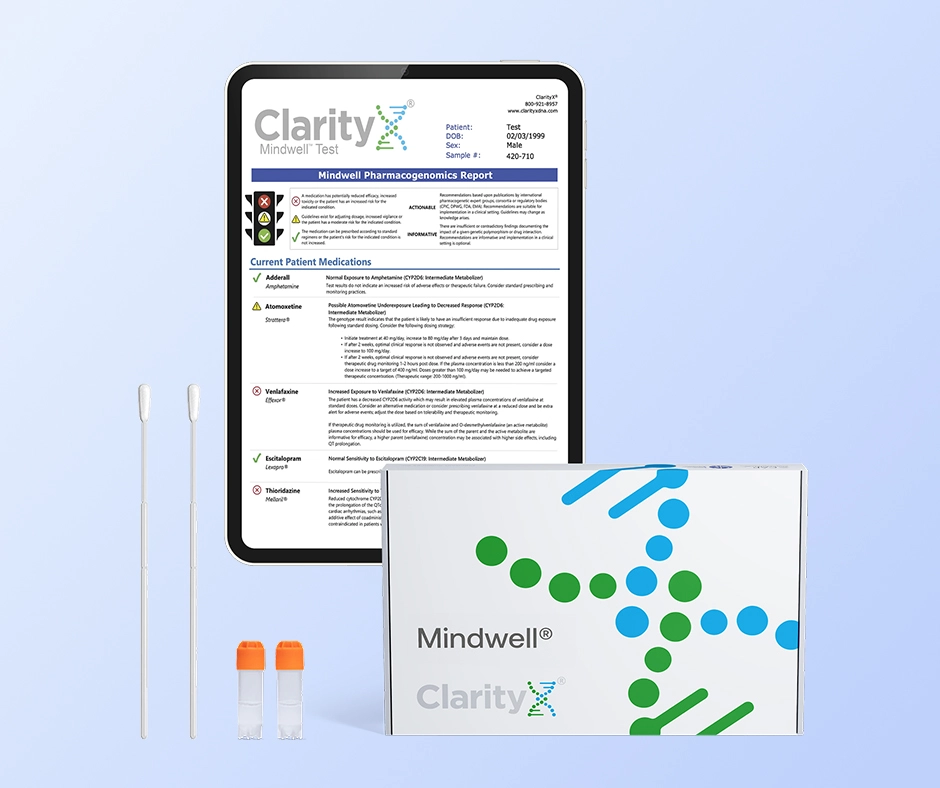
Genetic Testing and Its Benefits
To navigate these complexities and further personalize treatment, genetic testing for ADHD and depression medications provides a powerful, evidence-based tool. This approach, known as pharmacogenetic testing (PGx), analyzes how a person’s unique genetic makeup influences their response to different drugs. For instance, a single gene like CYP2D6 is critical for metabolizing both amphetamine-based stimulants (like Adderall) and numerous antidepressants. A PGx test can identify if a patient is a "poor" or "rapid" metabolizer, offering crucial guidance for selecting the right drug and dose to avoid side effects or treatment failure. By providing this biological roadmap, genetic testing helps clinicians tailor medication strategies more precisely from the start.
Clinicians should regularly monitor for changes in mood and side effects, adjusting the treatment plan as needed. Balancing benefits and risks, especially in adult patients, is key to optimizing outcomes and maintaining mental health stability.
Therapy and Behavioral Interventions
Therapy plays a vital role in managing both ADHD and depression. Cognitive behavioral therapy (CBT) is particularly effective, helping individuals challenge negative thoughts and build coping skills. Behavioral therapy can also improve organization and reduce impulsivity tied to ADHD symptoms.
Recommended interventions include:
- CBT for addressing depressive disorder and ADHD-related cognitive distortions
- Social skills training to support relationship building and reduce isolation
- Mindfulness-based stress reduction to manage emotional ups and downs
- Family therapy to enhance communication and provide support
These approaches can be used alongside medication or as a standalone strategy, depending on symptom severity. Engaging with therapy consistently helps people rebuild self-esteem, enhance daily functioning, and maintain long-term well-being.
Conclusion
Understanding the intricate relationship between ADHD and depression is crucial for effective management and treatment. These conditions often overlap in symptoms and challenges, which can make diagnosis more complex. Recognizing the emotional and behavioral differences between them is key to creating better outcomes. Additionally, untreated ADHD can increase the risk of developing or worsening depression, making early identification essential. If you suspect you or someone you know may be affected by these conditions, seeking professional help is a vital step. For personalized guidance—including options for pharmacogenetic testing—don’t hesitate to reach out for a free consultation with our expert team. Your mental health journey deserves both precision and care.
Frequently Asked Questions
What should I do if I think I have both ADHD and depression?
If you suspect you have ADHD and depressive symptoms, seek a full ADHD diagnosis and mental health assessment from a qualified professional. Early detection and targeted treatment of ADHD and depression can greatly improve your mental health and daily functioning.
Can a misdiagnosis affect how these conditions are treated?
Yes, misdiagnosis can lead to inappropriate ADHD treatment or missed depressive disorder management. Because these mental disorders share symptoms, accurate diagnosis is vital for selecting the right psychiatric interventions and avoiding complications in managing both conditions.
Are there therapies that help manage both ADHD and depression simultaneously?
Cognitive behavioral therapy and other behavioral therapy approaches are proven to address both ADHD symptoms and those of depressive episodes. Combined with medication, these therapies can help you manage day-to-day challenges and improve overall functioning.
References :
https://www.nimh.nih.gov/health/topics/attention-deficit-hyperactivity-disorder-adhd
https://www.mayoclinic.org/diseases-conditions/depression/symptoms-causes/syc-20356007
https://add.org/wp-content/uploads/2015/03/adhd-questionnaire-ASRS111.pdf
https://www.apa.org/depression-guideline/patient-health-questionnaire.pdf
https://adf.org.au/drug-facts/stimulants/
https://www.apa.org/ptsd-guideline/patients-and-families/cognitive-behavioral
https://www.healthline.com/health/behavioral-therapy
https://www.mayoclinic.org/diseases-conditions/depression/in-depth/antidepressants/art-20046273
https://www.drugs.com/bupropion.html
https://clarityxdna.com/blog/learn/cyp2d6-gene-plays-major-role-drug-metabolism/