Introduction
The human body is a complex and dynamic system where numerous chemical reactions take place continuously to maintain its functionality. One crucial aspect of these processes is drug metabolism, which involves the transformation of pharmaceutical compounds into active or inactive metabolites. Metabolism refers to how your body changes a medication to either make it more available or activate it; or, instead, make the medication less available by deactivating and improving the ability of your body to process and clear the medication.
An enzyme is a protein your body makes that actively changes other components in your body to a different form, for example, enzymes from your pancreas help to break down your food as part of the digestive process. Enzymes are crucial for life, helping with digestion, energy production, DNA replication, protein synthesis, drug metabolism and much more.
Among the various enzymes responsible for drug metabolism, CYP2C19 stands out as a pivotal player. This article explores the significant role of CYP2C19 in the body, its involvement in metabolizing specific medications, and the impact of pharmacogenetics on individual drug responses.
What does CYP2C19 do in the body?
Cytochrome P450 2C19 (CYP2C19) is a member of the cytochrome P450 enzyme family, which is primarily located in the liver but can also be found in other organs, such as the intestines. These enzymes play a vital role in the metabolism of a wide range of endogenous (made by our body) compounds, including fatty acids and steroid hormones, as well as various exogenous (foreign) substances, such as drugs and other medications.
CYP2C19 is responsible for the oxidation of many clinically significant medications, converting them into metabolites that are either more active or less active than the parent drug. The enzyme achieves this through a series of chemical reactions that add oxygen atoms to specific sites on the drug molecule. The resulting metabolites are then eventually excreted from the body through urine or feces. Importantly, CYP2C19 exhibits considerable genetic variability, leading to significant differences in drug metabolism among individuals, a phenomenon known as pharmacogenetics.
What medications are metabolized by CYP2C19?
CYP2C19 participates in the metabolism of a wide array of medications. CYP2C19 activity greatly influences drug response and therapeutic outcomes. Here are just some of the most notable medications that undergo CYP2C19-mediated metabolism include:
- Proton Pump Inhibitors (PPIs): PPIs are commonly prescribed for the treatment of acid-related gastrointestinal disorders such as peptic ulcers and gastroesophageal reflux disease (GERD). Individuals who have ultra-rapid metabolism with CYP2C19 may experience diminished drug efficacy, often requiring increased dosages. Common PPIs include omeprazole (Prilosec), esomeprazole (Nexium), pantoprazole (Protonix), lansoprazole (Prevacid), and others. PPIs all reduce acid in the stomach. Depending on your genetic makeup, one PPI may work better than another.
- Clopidogrel: Clopidogrel (Plavix) is an antiplatelet medication used to prevent blood clots in patients with cardiovascular diseases. CYP2C19 converts clopidogrel into its active form, and individuals with impaired CYP2C19 function may have reduced platelet inhibition, leading to an increased risk of cardiovascular events. If your genetic CYP2C19 gene fails to activate clopidogrel, then you are receiving this medication has no benefit. Genetic testing is recommended prior to starting antiplatelet treatment.
- Selective Serotonin Reuptake Inhibitors (SSRIs): There are many different SSRIs. Common examples include fluoxetine (Prozac), citalopram, escitalopram (Lexapro), paroxetine (Paxil), sertraline (Zoloft), and others. CYP2C19 metabolizes these medications and may lead to considerably different responses for the same medication in different people. How well your CYP2C19 enzyme works is unique to you. If an SSRI is not the best choice, there are multiple other options for treatment.
- Benzodiazepines: Diazepam (Valium) and clobazam (Onfi), used for anxiety and epilepsy, undergo CYP2C19 metabolism. Altered enzyme activity may alter drug clearance and efficacy, leading to potentially dangerous side effects with reduced benefit. Depending on your genetics, medications like clobazam may need to be greatly dose reduced for safety. The FDA recommends genetic testing prior to beginning clobazam treatment. Alternative benzodiazepines, such as lorazepam, alprazolam, and temazepam may be better alternatives for those who are CYP2C19 poor metabolizers, although other genes or health conditions need to be considered.
- Anticonvulsants: Phenytoin (Dilantin) and other anticonvulsants are metabolized by CYP2C19. Variability in enzyme function can lead to differences in drug levels and treatment outcomes for patients with epilepsy. Brivaracetam (Briviact) may require a dose reduction in patients who are CYP2C19 poor metabolizers according to the FDA. Often patients exhibit greater side effects in medications that are affected by their genes. Knowing ahead of time which medications may work best can improve patient care.
- Cyclophosphamide (Cytoxan), used to treat lupus, as well as many diverse kinds of cancer, requires activation by multiple enzymes including CYP2C19. Treatment response is highly dependent on your genetic profile.
Pharmacogenetics CYP2C19
Pharmacogenetics is the study of genetic variations that influence medicines. The gene that encodes CYP2C19 can have multiple changes. These changes have been broadly categorized into how they affect the function of the CYP2C19 enzyme. Called genetic polymorphisms, they can lead to five main phenotypes (or activities):
- Ultra-rapid metabolizer: Individuals have greater-than-normal CYP2C19 function. About 5% of people fall into this category. Avoiding, or dose reducing, lansoprazole, omeprazole, pantoprazole, and voriconazole may be necessary. Other medications may also be affected.
- Rapid metabolizer: Individuals have a slightly higher CYP2C19 function than normal, about 12 % of people. These patients may need to avoid amitriptyline, escitalopram and citalopram; and possibly others.
- Normal metabolizer: Individuals metabolize as expected. About 43% of people fall into this group. These patients can expect a normal response to these medications; however, responses still may vary due to other genetic or health variables.
- Intermediate Metabolizer: Individuals metabolize drugs somewhere between normal and poor metabolizers; about 30% of individuals fall into this category. Their CYP2C19 enzyme activity is reduced, leading to altered drug metabolism. Clopidogrel may not work in these patients. There may be other medications as well.
- Poor Metabolizer: Individuals have little or no working CYP2C19 and cannot process medications that require this pathway. About 10% of people are affected. Patients who have severely reduced function should avoid medications such as clopidogrel, amitriptyline, voriconazole, sertraline, citalopram, escitalopram and possibly others.
These genetic variations can significantly impact drug efficacy, safety, and side effect profiles. For example, poor metabolizers of clopidogrel are at a higher risk of stent thrombosis following coronary stent placement, highlighting the importance of pharmacogenetic testing in personalized medicine.
Certain medications affect how CYP2C19 works. These medications, although they may or may not rely on CYP2C19 for their own metabolism, can make the CYP2C19 activity change. Inhibitors, such as fluvoxamine, isoniazid, and ritonavir cause CYP2C19 metabolism to go down. Inducers, such as carbamazepine, phenytoin, and rifampin cause CYP2C19 metabolism to increase. Omeprazole and phenobarbital are highly affected by these medications and can also affect other medications.
Conclusion
CYP2C19 plays a crucial role in drug metabolism, influencing the efficacy and safety of various medications. This genetic variability among individuals can lead to significant differences in drug response, making pharmacogenetic testing an essential tool for personalized medicine. Understanding the interplay between CYP2C19 and drug metabolism not only enhances the effectiveness of pharmacotherapy but also minimizes the risk of adverse drug reactions. As research in pharmacogenetics continues to advance, healthcare providers can better tailor drug regimens to individual patients, ushering in an era of more precise and personalized healthcare.
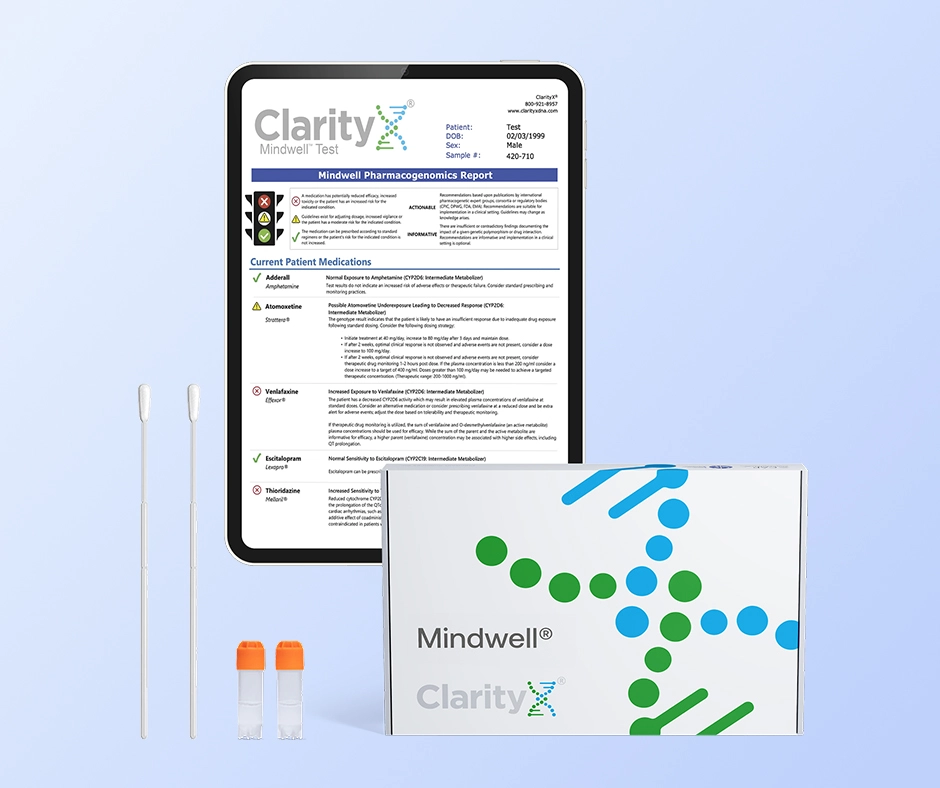
ClarityX provides pharmacogenomic testing to help you and your doctor move beyond trial and error and make better medication choices based on your genetic profile.
Resources:
- https://www.genome.gov/genetics-glossary/Enzyme
- https://www.frontiersin.org/articles/10.3389/fimmu.2018.00089/full
- https://files.cpicpgx.org/data/guideline/publication/PPI/2020/32770672.pdf
- https://files.cpicpgx.org/data/guideline/publication/clopidogrel/2022/35034351.pdf
- https://files.cpicpgx.org/data/guideline/publication/serotonin_reuptake_inhibitor_antidepressants/2023/37032427.pdf
- https://www.nature.com/articles/s41397-022-00267-7
- https://www.pharmgkb.org/labelAnnotation/PA166104884
- https://www.pharmgkb.org/labelAnnotation/PA166153492
- https://www.pharmgkb.org/pathway/PA145011115
- https://www.pharmgkb.org/pathway/PA165817070
- https://www.pharmgkb.org/chemical/PA449165
- cyclophosphamide: Dosing, contraindications, side effects, and pill pictures - epocrates online
- https://www.stjude.org/treatment/clinical-trials/pg4kds-pharmaceutical-science/implemented-genes/cytochrome-p450-2c19-cyp2c19.html