There are an estimated 350 million people all over the world that are debilitated by major depressive disorder (MDD).1 In the midst of the COVID-19 global pandemic it has been studied that the incidence of depression in the United States is 3 times higher compared to rates prior to the pandemic.2 COVID-19 has greatly impacted the global economy, quarantine has taken a negative toll on people’s mental health, and many have struggled to find treatments for their conditions. However, the number of people struggling with mental health has been growing long before the global pandemic. There are a wide variety of drugs that can be taken to help treat mental illness. How can someone determine which medication is right for them?
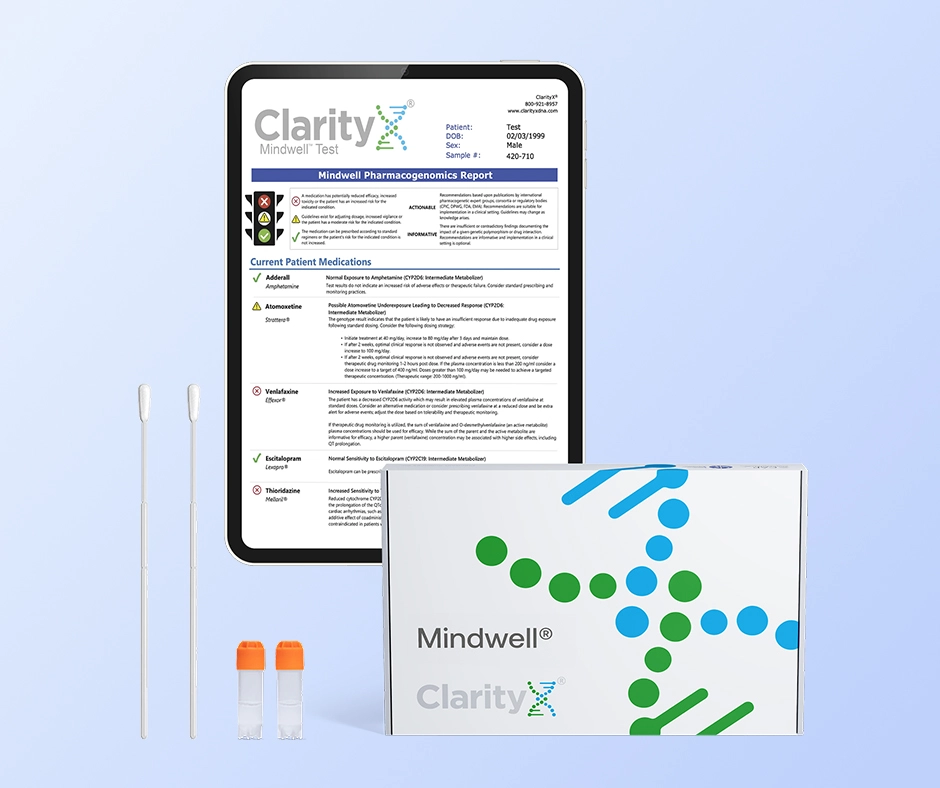
The market is saturated with a vast number of drugs to treat psychiatric conditions, and it can be very difficult to find the one that will work best for you. Even with the help of a doctor, it can still be a long and painful process to find the right treatment. Luckily, pharmacogenetic (PGx) testing can help with this. ClarityX® has a PGx test specifically designed to determine how someone may respond to mental health medications based on their genetics called Mindwell. 3
Genetic Testing for Antidepressants & Psychiatric Medications
What is Pharmacogenetic (PGx) Testing?
To comprehend genetics, there needs to be a basic understanding of DNA. It is easiest to think of DNA as a code that utilizes the letters A, C, G, and T to comprise its many genes. Different combinations of these letters signify the instructions those genes utilized to produce proteins in the body. Proteins are made up of amino acids sequenced from a corresponding gene. Proteins carry out many different functions of the body and one of those functions is the breakdown of medications (CYP450 enzymes). To put it simply, pharmacogenetic (PGx) testing evaluates someone’s genetic makeup to see if any variations or mutations in their genes can impact how their body responds to drugs. CYP450 enzymes are produced in the body from a unique genetic code of an individual. These CYP450 enzymes are responsible for eliminating or activating medications in the body. Having knowledge of any genetic abnormalities that can affect CYP450 enzymes can help mental health providers select the most appropriate medications for each patient. This new and exciting way of using PGx testing to determine which antidepressant to use is part of the precision medicine revolution in health care. Providers are working toward a more comprehensive approach to medicine so that the trial and error with patients’ medication selection will be a notion of the past. Ultimately, PGx testing can help prevent unwanted side effects and adverse events for their patients as well as save precious time and money by not initiating the right medication from the start. 4
There are typically five ways to identify pharmacogenomic phenotypes (labels) in PGx testing are as follows: Poor Metabolizer, Intermediate Metabolizer, Normal Metabolizer, Rapid Metabolizer, and Ultra-Rapid Metabolizer. These phenotypic labels can foreshadow how medications can be broken down in the body or activated. Low enzymatic activity may prevent a patient from metabolizing medications like antidepressants and antipsychotics. When the drugs remain in the system too long, they can cause serious side effects. In contrast, in those with high levels of enzymatic activity, medications can break down too quickly resulting in no therapeutic benefit.
How Pharmacogenetics (PGX) Testing Works for the Mindwell Test
The Mindwell test from ClarityX® provides a seamless in-home testing experience. Simply visit the website clarityxdna.com, select the Mindwell test option from the drop-down menu, and complete the checkout process. Once the kit is received follow the package instructions, perform a simple cheek swab, then mail the sample back using the prepaid envelope. The sample is then sent to the lab for processing and the results are received by the provider in 7-14 days on average. One of the most important facts about pharmacogenetic (PGx) testing is the results can be reevaluated for future medication changes as this test does not have to be repeated for those specific genes tested. Another key function of the Mindwell test is specific medications can be entered to be evaluated to see how an individual’s genetic makeup can affect those therapies. Pharmacogenetic (PGx) testing can provide a lifetime of knowledgeable decisions about medication selection for healthcare teams. When trial and error isn’t practical or simply too time-consuming and inconvenient, pharmacogenetic (PGx) testing for mental health medications can help providers prescribe proper dosages and determine which drugs will have the most benefit or potentially cause the most side effects. Having the proper mental health medication along with its appropriate dosage can have a huge impact on those with mental illnesses. It’s well documented that antidepressants can take up to four to six weeks before they provide any relief to mental health conditions like depression. More often than not patients will stop taking antidepressants usually within a few months because of negative side effects or the medication wasn’t working at all to resolve their symptoms. Patient’s abruptly stopping their mental health medications can produce other problems on top of their current mental health diagnosis such as withdrawal symptoms. Many of these complications can be avoided by simply having knowledge of how a patient uniquely reacts to mental health medications.
Examples of Gene Variations Affecting Antidepressants
There are currently over 40 antidepressants that are available on the market to treat mental health conditions. In many situations, patients may be required to take more than one psychiatric medication to treat their particular condition. Unfortunately, the journey for most people when finding the right medications with accurate doses to optimize their therapy can be a daunting task for both the health care practitioner and the patient. For example, there are two CYP450 enzymes that can be impacted by an individual’s genetics affecting how medications react in the body. The two enzymes are CYP2D6 and CYP2C19. 5
According to the Clinical Pharmacogenetics Implementation Consortium (CPIC), there is meaningful, well-documented evidence to support the findings around the enzymes CYP2D6 and CYP2C19 being affected by genetic variations. The genetic variations of these enzymes have been clinically shown to alter the effects of serotonin reuptake inhibitors (SSRIs) and tricyclic antidepressants (TCAs), which are both common first-line therapies prescribed when treating mental health conditions. Patients potentially could experience treatment failure if these genetic variations are not identified prior to initial treatments. For example, of patients diagnosed with major depressive disorder, approximately 50% have the potential to fail initial therapy with an SSRI. In addition, nearly 25,000 patients annually in the United States will need to go to the emergency department due to adverse events caused by antidepressants. 6
SSRI’s Affected by Genetic Variations in CYP2C19
Three common SSRI treatments in mental health are citalopram (Celexa), escitalopram (Lexapro), and sertraline (Zoloft). These medications can be strongly affected by patients that carry the genetic variant to make the enzyme CYP2C19 have ultrarapid metabolism. Having CYP2C19 ultrarapid metabolism with these medications can cause a person to not have any therapeutic benefit because the drugs are eliminated out of the body too quickly. Conversely, if a patient is found to be a poor metabolizer of CYP2C19, the patient may experience a buildup of the medication in the system and experience side effects or adverse events. 7
TCA’s Affected by Genetic Variations in CYP2D6
TCAs are not commonly initially prescribed in mental health treatment plans due to their increased risks of side effects. However, nortriptyline (Pamelor) and amitriptyline (Elavil) are still commonly seen in practice today with the most pharmacogenomic supporting evidence for dosing adjustments. In the situation of CYP2D6 ultrarapid metabolism being found in a PGx testing result for a patient, it is likely this patient will receive no therapeutic benefit from nortriptyline or amitriptyline since they would be eliminated from the body so quickly. Conversely, if CYP2D6 is found to have poor metabolism a patient may experience side effects or adverse events due to a buildup of the medication in the body. 8
Mindwell Test Benefits
There are so many antidepressants and psychiatric medication options. It can be overwhelming. Choosing the wrong one can lead to a host of unpleasant side effects and sometimes even the original problem remains unresolved. ClarityX® Mindwell test can help patients find the right mental health medication and ultimately improve their life. The Mindwell test can provide clear insight into which medications will work best for patients suffering from mental health conditions such as clinical depression, anxiety disorders, bipolar disorder, ADHD/ADD, OCD, PTSD, schizophrenia, opioid withdrawal, and pain management. Pharmacogenomics is the way of the future and can provide a lifetime of knowledgeable medication decisions for providers and patients.
Citations
[1] Corponi, F., Fabbri, C., & Serretti, A. (2019). Pharmacogenetics and Depression: A critical perspective. Psychiatry Investigation, 16(9), 645–653. https://doi.org/10.30773/pi.2019.06.16
[2] Ettman, C. K., Abdalla, S. M., Cohen, G. H., Sampson, L., Vivier, P. M., & Galea, S. (2020). Prevalence of depression symptoms in US adults before and during the COVID-19 pandemic. JAMA Network Open, 3(9). https://doi.org/10.1001/jamanetworkopen.2020.19686
[3] https://www.clarityxdna.com/clarityx-mental-wellness-test/
[4] https://www.pharmgkb.org/whatIsPharmacogenomics
[5] Corponi, F., Fabbri, C., & Serretti, A. (2019). Pharmacogenetics and Depression: A critical perspective. Psychiatry Investigation, 16(9), 645–653. https://doi.org/10.30773/pi.2019.06.16
[6] Hicks, J. K., Bishop, J. R., Sangkuhl, K., Müller, D. J., Ji, Y., Leckband, S. G., Leeder, J. S., Graham, R. L., Chiulli, D. L., LLerena, A., Skaar, T. C., Scott, S. A., Stingl, J. C., Klein, T. E., Caudle, K. E., & Gaedigk, A. (2015). Clinical pharmacogenetics implementation consortium (CPIC) guideline forcyp2d6andcyp2c19genotypes and dosing of selective serotonin reuptake inhibitors. Clinical Pharmacology & Therapeutics, 98(2), 127–134. https://doi.org/10.1002/cpt.147
[7] Hicks, J. K., Bishop, J. R., Sangkuhl, K., Müller, D. J., Ji, Y., Leckband, S. G., Leeder, J. S., Graham, R. L., Chiulli, D. L., LLerena, A., Skaar, T. C., Scott, S. A., Stingl, J. C., Klein, T. E., Caudle, K. E., & Gaedigk, A. (2015). Clinical pharmacogenetics implementation consortium (CPIC) guideline forcyp2d6andcyp2c19genotypes and dosing of selective serotonin reuptake inhibitors. Clinical Pharmacology & Therapeutics, 98(2), 127–134. https://doi.org/10.1002/cpt.147
[8] Hicks, J. K., Sangkuhl, K., Swen, J. J., Ellingrod, V. L., Müller, D. J., Shimoda, K., Bishop, J. R., Kharasch, E. D., Skaar, T. C., Gaedigk, A., Dunnenberger, H. M., Klein, T. E., Caudle, K. E., & Stingl, J. C. (2017). Clinical pharmacogenetics implementation consortium guideline (CPIC) for cyp2d6 and cyp2c19 genotypes and dosing of tricyclic antidepressants: 2016 update. Clinical Pharmacology & Therapeutics, 102(1), 37–44. https://doi.org/10.1002/cpt.597