Key Highlights
- Blood thinners, also known as anticoagulants, play a key role in stopping blood clots, heart attacks, and strokes from happening.
- Among these medications are clopidogrel (Plavix) and warfarin. They're both commonly used but work differently to prevent clotting.
- Clopidogrel stops platelets from clumping together, and warfarin works by blocking the production of substances that cause clotting.
- Choosing between them involves considering each person's unique health background and the potential benefits or risks associated with each option.
- Antiplatelet medications like Plavix are often prescribed after a heart attack or stroke. In contrast, anticoagulants like warfarin are often prescribed to reduce the risk of blood clots in other areas, such as the legs or lungs. In some situations, both types of medications may be recommended for additional support.
- Plavix depends on CYP2C19 enzymes to be converted to an active form that helps prevent clots. Genetic testing can help predict whether Plavix is likely to be effective.
- With any blood thinner treatment comes the need for regular check-ups to ensure everything is going smoothly and safely.
Introduction
Blood thinners, including Plavix and Warfarin, are essential for treating conditions like atrial fibrillation and heart disease. Understanding how they work and what makes them different helps ensure the medical treatment works well.
Both of these drugs stop clots from forming but have different side effects and safety concerns. When choosing between them, things like specific patient needs, how other medicines might react with them, and their cost matter a lot. Healthcare providers have a big job in keeping an eye on how the treatment is going and teaching patients so that everything goes as planned.
Understanding Blood Thinners: An Overview
Blood thinners, or anticoagulants, are important for stopping blood clots from forming and maintaining a healthy blood supply. They're often given to people with conditions like atrial fibrillation, heart attack, and deep vein thrombosis. By affecting how the blood clots, these meds help lower the chance of having an ischemic stroke, which can lead to brain tissue death from brain cell damage or death, or a pulmonary embolism, where an artery ruptures and blocks blood flow to the lungs. Understanding the classic symptoms and warning signs of a pulmonary embolism is critical. These include:
- Chest pain.
- Shortness of breath.
- Pain that radiates to other areas of the body.
In addition, the warning signs of a stroke or transient ischemic attack include:
- Difficulty speaking.
- Weakness
- Numbness.
- Facial droop
- Disorientation.
- Agitation.
Identifying these quickly and seeking immediate medical attention can help potentially prevent serious complications.
For those taking blood thinners, it's vital to get checked out regularly because there's a significant risk of severe bleeding if something goes wrong, such as a blood vessel rupture.
The Importance of Blood Thinners in Preventing Clots
For people who are at a higher risk because they have things like atrial fibrillation or a history of heart attack, blood thinners can be life-saving. They stop clots from forming by keeping platelets from sticking together and ensuring blood doesn't get blocked in the vessels. This can help avoid serious problems such as pulmonary embolism or ischemic stroke.
When it comes to folks dealing with a risk of deep vein thrombosis, taking these medications is crucial for maintaining good blood flow and preventing any dangerous clots from popping up, especially for those with a family history of blood clots.
How Blood Thinners Work in the Body
Medications like Plavix and warfarin are known as blood thinners. They work by stopping the body from forming clots. By focusing on different parts of the clotting process, such as platelet aggregation or certain clotting factors, these drugs help prevent blood clots from happening.
The Basics of Plavix (Clopidogrel) and Warfarin
Plavix, which you might also hear called clopidogrel, and warfarin are two blood thinners doctors often give to their patients. Plavix helps by stopping blood platelets from clumping together and making clots. This is helpful for people with acute coronary syndrome (i.e., heart attack) and peripheral arterial disease.
Conversely, warfarin interferes with how vitamin K works in your body, which changes how well your blood can form clots. Knowing what each of these does is super important when figuring out the best way to treat different health issues.
What is Plavix? Understanding its Role and Mechanism
Plavix, known as clopidogrel bisulfate, is an antiplatelet medication used to prevent blood clots in patients with conditions such as acute coronary syndrome, peripheral vascular disease, and myocardial infarction. It works by inhibiting platelet aggregation, making it a vital medication for those at risk of heart attacks or strokes.
Plavix depends on a liver enzyme called CYP2C19 to be converted to an active form. Some individuals produce less of this enzyme, leaving Plavix less effective for preventing clots. Genetic testing can help predict this and is highly valuable in determining whether an individual will likely benefit from Plavix therapy.
What is Warfarin? How it Differs from Plavix
Warfarin is a medicine that stops blood clots by blocking clotting factors in your body that need vitamin K to work. On the other hand, Plavix helps prevent clots by keeping platelets from sticking together. With warfarin, you have to check in with your doctor often because getting the dose just right can be tricky. But Plavix makes it easier to know how it will affect you without needing as many follow-up checks.
Key Differences Between Plavix and Warfarin
Plavix (clopidogrel) and Warfarin work in different ways to prevent blood clots. Plavix stops platelets from sticking together, while Warfarin affects clotting factors that need vitamin K to work properly.
When it comes to side effects, taking Plavix may be less likely to cause severe bleeding than warfarin; the latter needs close watching because of its high risk of bleeding.
Also, with warfarin, you have to be careful about what food and medicine you mix it with—something that's not as much of a worry with Plavix. However, the risk of bleeding with Plavix is still significant. Knowing these differences is key when choosing the right blood thinner for someone based on their needs.
Mechanism of Action: How Each Drug Prevents Blood Clots
Plavix, also known as clopidogrel, stops platelets from sticking together because it blocks ADP receptors. This action lowers the chance of clots forming.
On the other hand, warfarin interferes with clotting factors that rely on vitamin K . By doing this, it takes longer for blood to clot and helps prevent clots from happening in the first place.
While Plavix focuses on platelet aggregation at one stage of clot formation, Warfarin targets proteins involved in clotting at a different step, making each an effective blood thinner. Depending on individual patient needs, both medications may be recommended for use at the same time.
Side Effects and Safety Profiles
Plavix and Warfarin work well to thin the blood, but they have some differences when we look at their side effects. Both medications are associated with significant bleeding risks, some of which can be dangerous or fatal. Also, if you're on Warfarin, you'll need to get checked out regularly because it's crucial to get the dose just right. Knowing these differences is important in choosing which one is better for you. It’s always best to talk things over with your doctor so that together, you can make an informed choice based on what’s going on with your health.
Similarities Between Plavix and Warfarin
Plavix and Warfarin are both important medications that help prevent blood clots, making them useful for people with conditions like atrial fibrillation or those who've had a heart attack. With these drugs, there's always a chance of bleeding, so it's vital to keep an eye out for bruising or bleeding.
Doctors pay close attention when someone is taking these medicines because of the possible side effects and the need for ongoing medical advice. Even though Plavix and Warfarin have their differences, they're both vital in keeping the cardiovascular system healthy and have similar risk factors, including interactions with other drugs that increase the risk of bleeding.
Common Conditions Treated by Plavix and Warfarin
Plavix (Clopidogrel) is often given to folks dealing with health issues like peripheral arterial disease, ischemic stroke, and acute coronary syndrome - which includes unstable angina marked by acute chest pain and classic heart attack. It helps stop blood clots from forming after someone has had a stent placed or a heart attack.
Warfarin is commonly used in treating deep vein thrombosis and pulmonary embolism. Additionally, it’s often prescribed for patients with atrial fibrillation or artificial heart valves to reduce the risk of strokes. Warfarin is also sometimes used for individuals with peripheral arterial disease.
Monitoring and Management of Treatment
Keeping an eye on things is very important when taking blood thinners such as Plavix and Warfarin. This helps make sure they're working right and not causing any harm. Doctors check your blood levels and blood pressure, tweak how much medicine you take, and look out for any bad reactions. It's also key that patients learn about sticking to their treatment plan and spotting early warning signs of more serious problems by reporting concerns with bruising or bleeding.
The goal here is to find the perfect balance between preventing clots and avoiding too much bleeding. By staying on top of monitoring and managing treatment, we can get the best results from therapy while keeping risks low.
Factors to Consider When Choosing Between Plavix and Warfarin
There may be a clear recommendation for some conditions to use one medication over the other, but there are instances where either medication could be considered. When choosing between Plavix and Warfarin for someone, it's vital to consider unique health issues like liver problems or how much vitamin K they get in their diet. We also have to consider how likely they are to bleed and whether any other medicines they're taking might not mix well with these blood thinners. The cost and whether these medications are easy to get hold of can't be ignored either, especially if the person needs them for a long time.
Patient-Specific Factors and Drug Interactions
When picking blood thinners like Plavix or warfarin, the decision hinges on the condition or conditions being treated and how other medicines might mix with each choice. There are also different options, including some newer ones called direct oral anticoagulants (DOACs), that could work better depending on the person's unique situation.
Looking closely at each patient’s health background, lifestyle, and any possible drug interactions before choosing which blood thinner to use is best. This way of tailoring treatment helps make sure patients get the most benefit while keeping risks low.
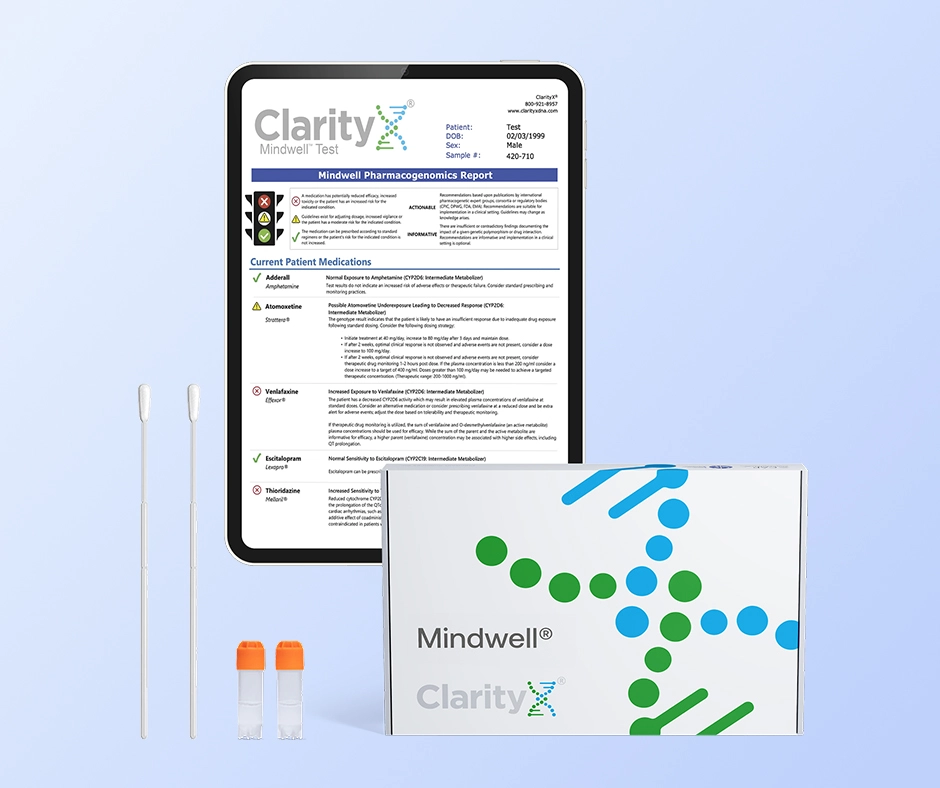
Pharmacogenomic Testing
Pharmacogenomic testing is a precision medicine tool that analyzes your DNA to predict how your body will process and respond to specific medications. By examining genetic variants primarily those affecting liver enzymes the test reveals if you are likely to metabolize a drug too slowly (increasing the risk of severe side effects) or too quickly (making the medication ineffective).
This genetic insight allows doctors to move away from a "trial and error" prescribing method, helping them select the right drug and the right dose from the start to maximize treatment success while minimizing adverse reactions.
Cost Considerations and Accessibility
When picking a blood thinner, thinking about how much it costs and how easy it is to get are key points. In the United States, what you pay for healthcare can change from one place to another, making some drugs easier on your wallet or simpler to find than others. Warfarin often costs less because it's been widely available for an extended time, but keeping up with its needed checks and changing doses could increase its overall price.
Clopidogrel, the generic for Plavix, is widely available and can help improve out-of-pocket costs. It may be less expensive overall because it requires fewer frequent follow-up appointments. Reaching pharmacies and doctors easily matters because not everyone can easily access certain medicines or check-up services. It’s smart to talk over these money and access worries with your doctor so you can choose what works best for you.
The Role of Healthcare Providers in Managing Treatment
Healthcare providers must determine which medication is best for a patient, considering their health history and current condition. Providing a complete and accurate history is vital, along with continuing to communicate any potential concerns like bleeding or bruising. If needed, healthcare providers might change the dose or try a different type of blood thinner based on regular check-ups.
Regular Monitoring and Dosage Adjustments
Monitoring and tweaking the dose as needed is critical for folks taking blood thinners, especially warfarin. People using warfarin need to check their blood often so doctors can look at the International Normalized Ratio (INR). The INR helps determine how fast your blood clots, and keeping this number in a specific range matters a lot, especially for those with liver disease or other health issues that could affect the effect of warfarin. Frequent blood tests are crucial for monitoring the effect of warfarin and adjusting dosages accordingly. It’s important to listen closely to healthcare provider advice and make regular visits to check your blood levels. If there needs to be any change in what you're taking or how much, always do that with a doctor's guidance so you don't run into problems like too much bleeding or increasing your risk of clotting.
The Importance of Patient Education and Compliance
For people taking blood thinners, knowing what they're taking and following their doctor's advice is vital. It's all about understanding the good things these meds can do for you and being aware of any risks.
The American Heart Association, along with other trusted groups, has a lot of information to help people figure out the best way to handle their treatment. Taking your medicine just as prescribed - the right amount at the right time - is critical to keeping everything working smoothly and avoiding any unwanted problems. If anything feels off or side effects worry you, getting in touch with your healthcare provider fast is crucial. Being open and involved in your treatment can make a difference in how well these blood thinners work.
When considering treatment options your genetics can also play a vital role in determining which medications will be best suited for you. A simple test can help reduce the trial and error process associated with finding the right medication. Find out more by visiting www.clarityxdna.com
Conclusion
To wrap it up, deciding if Plavix or Warfarin is better for you comes down to really understanding how they work, what side effects they might have, and whether they're a good match based on your own health. Both medications are great at stopping blood clots, but picking the right one involves looking closely at things like the current condition or any other conditions you might have and how these drugs could mix with others you're taking.
Doctors play a key role in monitoring everything and teaching patients to ensure the treatment works as well as possible. Choosing between Plavix and Warfarin should be something you do after getting advice from medical experts so that it's safe and does its job in preventing clotting issues.
Frequently Asked Questions
Can Plavix and Warfarin be Used Interchangeably?
Plavix and warfarin are two blood thinners that shouldn't be swapped without a doctor's advice. They work in different ways; one can be preferred over the other depending on the managed condition. When deciding which one to use, doctors consider what's unique about the patient, how other medicines might react with them, and what they're hoping to achieve with treatment. With all these factors in mind, healthcare professionals can pick the most appropriate blood thinner after looking into each patient’s situation and considering potential drug interactions.
How Do I Know Which Blood Thinner is Right for Me?
To determine which blood thinner is best for you, your doctor needs to look closely at your past health issues, what could make you more likely to have problems like clots, and the specific health condition you're dealing with. If you've got something like atrial fibrillation or a high chance of clotting, these are key things they'll think about. They also need to watch out for how different medicines might react with each other when choosing the right blood thinner for your situation. It's really important that you talk openly with healthcare providers and ask questions so that together, you can choose the treatment plan that makes the most sense.
References
https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=558b7a0d-5490-4c1b-802e-3ab3f1efe760
https://medlineplus.gov/druginfo/meds/a682277.html
https://dailymed.nlm.nih.gov/dailymed/drugInfo.cfm?setid=de8b0b67-eb25-4684-83b5-7ad785314227
https://www.accessdata.fda.gov/drugsatfda_docs/label/2010/020839s048lbl.pdf
https://pubmed.ncbi.nlm.nih.gov/37471501/
https://pubmed.ncbi.nlm.nih.gov/38033089/
https://pubmed.ncbi.nlm.nih.gov/34024117/
https://pubmed.ncbi.nlm.nih.gov/38752899/
https://clarityxdna.com/blog/learn/cyp2c19-the-gene-drug-metabolism/
https://clarityxdna.com/blog/genetic-testing-for-medication-efficacy/