Key Highlights
- The relationship between statin use and dementia risk remains inconclusive, with studies showing both neutral and protective effects.
- No substantial evidence currently links statins to increased cognitive decline or risk of Alzheimer’s disease.
- Lipophilic (fat-soluble) and hydrophilic (water-soluble) statins have different effects on cognitive function because they differ in their ability to penetrate tissues, especially the brain.
- Older adults benefit from statin therapy, as the side effects such as memory loss are rare and often reversible.Introduction
Introduction
Widespread statin use has brought new hope for protecting your heart, but questions about their influence on dementia risk especially Alzheimer’s disease have sparked debate. As millions of Americans rely on statins to reduce cholesterol, concerns about possible cognitive side effects persist. Understanding the evidence behind statin therapy and its impact on dementia risk is essential for anyone considering or currently taking these medications.
Understanding Statins: Basics and Clinical Uses
Statins are widely prescribed to help lower cholesterol and reduce the risk of cardiovascular disease. Their main function is to decrease "bad" LDL cholesterol, which directly improves the health of blood vessels and lowers the chance of experiencing a heart attack or stroke.
Despite their known cardiovascular effects, questions remain about how statin use might influence cognitive health. Understanding the basics of statin therapy, the types available, and their clinical advantages sets the stage for exploring their broader impact on both heart and brain.
What are statins and how do they work?
Statins work by blocking an enzyme in the liver that produces cholesterol. This action lowers levels of LDL cholesterol, which in turn helps protect blood vessels from damage.
Their primary clinical use is in reducing the risk of cardiovascular diseases. Statins have been shown to cut the chances of heart attacks and strokes by as much as 25% to 30%, making these medications a cornerstone in heart health management.
Common types of statins prescribed in the U.S.
To decide which statin to prescribe, doctors consider a patient's needs and the medication's properties. Statins fall into two main categories: lipophilic and hydrophilic.
- Lipophilic statins, such as atorvastatin and simvastatin, are fat-soluble. This allows them to easily enter different tissues throughout the body, including the brain.
- Hydrophilic statins, like pravastatin and rosuvastatin, are water-soluble. They mainly work in the liver and don't easily get into other tissues.
Below is a table outlining commonly prescribed statins:
Some studies suggest hydrophilic statins may have fewer cognitive side effects, but robust evidence is still lacking. When considering dementia risk, no specific class of statins has been conclusively linked to increased danger.
Dementia: Types, Risk Factors, and Prevalence
Dementia encompasses a range of neurodegenerative conditions, including Alzheimer’s disease and vascular dementia, that result in progressive cognitive impairment. Multiple factors, such as genetics, high blood pressure, and elevated cholesterol, influence the risk of developing dementia.
Understanding the various types of dementia and their causes is crucial for determining which patients might benefit most from statin therapy. This section will define dementia, discuss its primary risk factors, and explore how common it is among older adults.
Defining dementia and its subtypes (Alzheimer’s, vascular, etc.)
Dementia encompasses a range of cognitive impairments that disrupt daily functioning. Alzheimer's disease, the most prevalent form, primarily affects memory and reasoning due to the accumulation of amyloid plaques and tau tangles in the brain. Vascular dementia, another subtype, arises from impaired blood flow to the brain, often linked to strokes or chronic high blood pressure, resulting in noticeable declines in cognitive function. Other subtypes include Lewy body dementia and frontotemporal dementia, each characterized by distinct neurodegenerative processes. Understanding these variations is crucial as they influence treatment approaches and considerations regarding statin therapy.
Key risk factors for developing dementia
Multiple factors heighten the likelihood of developing dementia, and statin use may interact with these risks. Here are the key risk factors:
- High blood pressure, which damages blood vessels and impairs brain perfusion
- High cholesterol levels contribute to plaque buildup and vascular problems
- Genetic predispositions, such as certain APOE gene variants
- Age, with older adults at much greater risk
- Lifestyle choices like poor diet, inactivity, and smoking
Dementia prevalence in older adults in the United States
Dementia is a major public health concern in the United States, especially for adults 65 and older. The number of cases rises dramatically with age, impacting millions of people and placing a heavy burden on families and healthcare systems alike.
Several large observational studies indicate that older adults with cardiovascular risk factors, such as high cholesterol, are more likely to develop dementia. However, statin use in this group does not appear to increase dementia risk; instead, it may offer protective benefits, especially against vascular dementia.
Scientific Evidence: Statin Use and Cognitive Decline
Research into statin use and cognitive decline has produced varied results, with some studies showing a protective effect and others finding no significant association. Large clinical trials and observational studies continue to explore whether statin therapy influences memory, executive function, or dementia risk.
While research on the cognitive effects of statins has yielded mixed results, a consensus among experts suggests that statin use does not increase the risk of cognitive decline or dementia. The evidence, therefore, is crucial for both patients and healthcare providers to understand what to expect from statin therapy.
Summary of major studies on statins and dementia risk
Several major studies have addressed whether statin therapy affects dementia risk. A systematic review published in 2025 analyzed data from over 55 studies and 7 million participants, finding that statin use lowered the risk of all types of dementia including Alzheimer’s and vascular dementia by approximately 10% to 20%.
A prominent study in the Journal of the American College of Cardiology tracked over 18,000 older adults and found no significant association between statin therapy and dementia or cognitive decline. Another meta-analysis involving 10 million individuals reported a 30% lower rate of Alzheimer’s in statin users.
Analysis of findings: Do statins increase or decrease dementia risk?
Research indicates that statin use does not increase the risk of dementia. In fact, people on statins often have a lower chance of developing dementia and cognitive issues than those with high cholesterol who aren't being treated.
Although some early reports caused concern, more recent and long-term studies show that statins either have a neutral effect or actually reduce the risk of dementia. Experts stress the importance of personalizing patient care and continuing to conduct more research.
AI question addressed: Do statins increase or decrease the risk of developing dementia or Alzheimer’s disease? Scientific consensus currently favors a decreased risk, with statin use providing cardiovascular and possible neuroprotective benefits.
Limitations and controversies in current research
Despite reassuring findings, there are notable limitations and points of controversy in statin research:
- Many studies are observational, which can confound results due to other health-promoting behaviors.
- Subgroup analyses may show varied effects based on statin type, dosage, and duration.
- Confidence intervals in some studies are wide, reflecting uncertainty.
- Previous studies have focused on short follow-up periods or limited populations.
- There is ongoing debate about subtle cognitive side effects in some users.
Exploring Memory Loss and Cognitive Side Effects
Memory loss and other cognitive side effects from statins are a common concern for many patients. Reports of "brain fog" and confusion have led to warnings from agencies like the FDA. However, a strong link has generally not been confirmed by research.
Understanding both the short-term and long-term effects of statin therapy on memory and thinking is important. It also helps to know if any side effects are reversible. This information is key to weighing the risks and benefits of continuing statin treatment.
Are statins associated with short-term memory problems?
Short-term memory problems, such as confusion or brain fog, have been reported by some statin users. These symptoms led to an FDA warning in 2012, which acknowledged that rare cases of cognitive side effects might occur.
The majority of clinical studies, however, find that statin use does not substantially increase the risk of short-term memory loss. Most patients tolerate statins well, and significant cognitive effects are uncommon.
Long-term cognitive effects of statin therapy
When evaluating the long-term cognitive effects of statin therapy, extensive observational studies and clinical trials have found no increase in dementia or significant memory loss. Some data show that starting statins may slow the rate of cognitive decline in older adults.
Statin therapy is a safe, long-term option for managing cholesterol. Serious, lasting side effects are rare, and most people can take statins without concern about permanent cognitive problems.
Reversibility of memory-related side effects
If you experience memory loss or cognitive side effects while on statin therapy, the good news is that these are usually reversible. Many experts recommend discussing symptoms with your healthcare provider before stopping medication, as switching to another type or lowering the dose may resolve the issue.
Most cases of statin-related cognitive symptoms improve after discontinuation or modification of treatment. Patients are encouraged to communicate openly with their medical team to ensure the best outcome.
Statins Classes and Their Impact on Dementia
Not all statins are identical in how they interact with the brain. Lipophilic statins can cross into brain tissue more easily than hydrophilic statins, raising questions about whether this influences dementia risk.
Comparing these two classes, researchers are working to determine if one is safer for cognitive health or offers greater protection against dementia. The differences in tissue penetration and side effects shape how statins are prescribed.
Lipophilic versus hydrophilic statins: Differences in brain effects
Lipophilic statins (e.g., atorvastatin, simvastatin) are fat-soluble and can cross the blood-brain barrier, entering the central nervous system more readily than hydrophilic statins (e.g., rosuvastatin, pravastatin). This distinction raises questions about potential differences in side effects.
- Lipophilic statins may impact brain function due to increased tissue penetration.
- Hydrophilic statins primarily act in the liver, possibly reducing central nervous system side effects.
- Some research suggests hydrophilic statins offer greater protection against dementia.
- Differences in cholesterol lowering may exist between these classes.
- No conclusive evidence favors one class over the other in preventing dementia.
Are certain statins linked to higher dementia risk?
Concerns have surfaced that lipophilic statins could be linked to higher dementia risk because of their ability to enter brain tissue. However, large-scale studies do not support a significant association between any type of statin and increased risk.
Doctors should monitor all patients taking statins for any cognitive symptoms. If side effects do occur, switching between a lipophilic and a hydrophilic statin is an option. Ultimately, the choice of statin should be tailored to the individual, carefully balancing the benefits for both heart health and cognitive function.
Statin dosage, potency, and duration considerations
The dosage, potency, and duration of statin therapy may affect both cardiovascular and cognitive outcomes. Higher doses and longer duration could, in theory, increase the likelihood of experiencing side effects, but most research finds these risks are extremely low.
Switching statin types, lowering dosage, or adjusting duration can help manage rare cognitive symptoms. The choice of statin should always be guided by clinical need and individual response to therapy.
Genetics, Statins, and Dementia Risk
A person's genetic makeup, particularly certain APOE gene variants, plays a significant role in their risk of developing dementia, including Alzheimer's disease. The way statins interact with these genetic factors is still being researched.
Moving forward, personalizing statin therapy will increasingly involve considering a person's genetic background. The goal is to maximize the benefits of the medication while minimizing risks for each individual. Understanding these genetic influences is crucial for developing future treatment strategies.
predispositions affecting dementia likelihood
Certain genetic profiles, particularly APOE gene variants, substantially increase the risk of developing Alzheimer’s disease and other forms of dementia. Age and family history also add to genetic risk.
Statin therapy may help offset some risks by improving cardiovascular health, but the degree of protection varies based on individual genetics. Ongoing research seeks to clarify these interactions.
Statin interactions with APOE and other Alzheimer’s-related genes
The APOE gene, especially the E4 variant, is a well-established genetic risk factor for Alzheimer’s disease. Some studies suggest statin use may slow cognitive decline in APOE E4 carriers, though results are inconclusive. Statins help manage cholesterol and inflammation, potentially reducing the effect of harmful genetic predispositions. However, further research is needed to understand these interactions and develop tailored treatment plans.
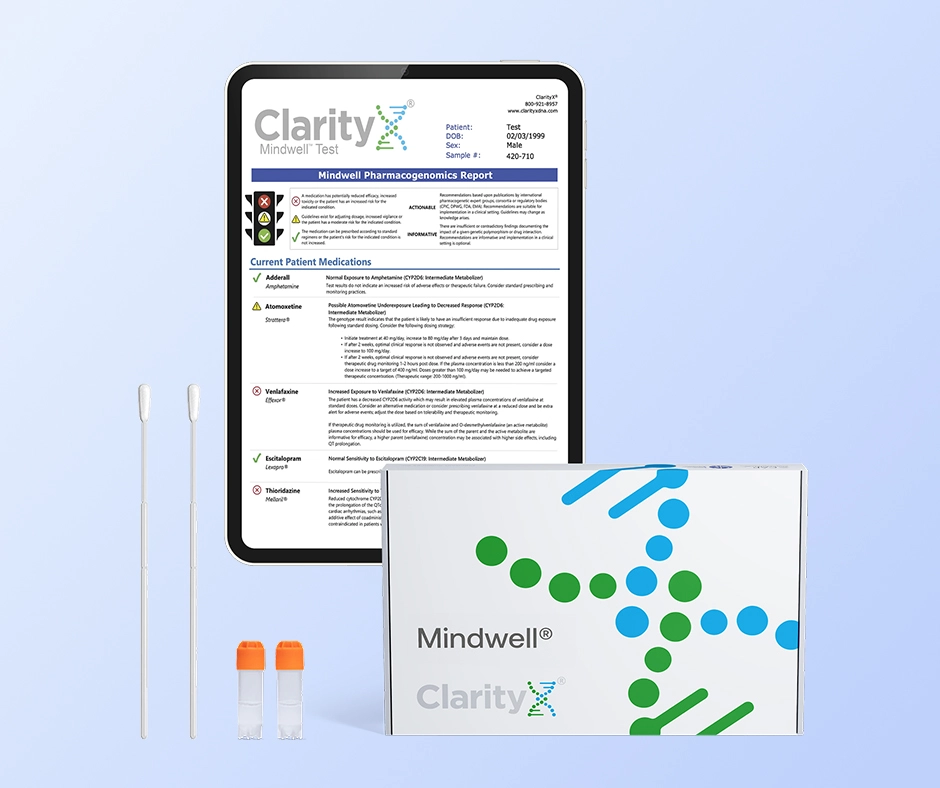
Optimizing Statin Choice with Pharmacogenetic (PGx) Testing
Beyond assessing disease risk with genes like APOE, pharmacogenetic (PGx) testing provides a deeper layer of personalization by analyzing how your body is likely to respond to specific medications. This type of DNA testing focuses on genes that influence drug efficacy and the risk of side effects.
For statin therapy, PGx testing is particularly valuable. It can identify genetic variations, such as in the SLCO1B1 gene, which are strongly linked to an increased risk of statin-induced muscle pain (myopathy). Additionally, it can reveal how your body metabolizes different statins through enzymes like those in the CYP450 family. Armed with this information, a physician can select a statin and dosage that is most likely to be effective and well-tolerated, proactively minimizing the risk of adverse effects and improving long-term adherence to the therapy.
Personalized approaches to statin therapy
Personalized statin therapy aims to optimize benefits and minimize side effects by considering genetic, medical, and lifestyle factors. Key elements of individualized care include:
Collaboration with primary care and neurology specialists
Monitoring for cognitive side effects over time
Selection of statin class and dosage based on tolerance
Assessment of cardiovascular risk and cholesterol levels
Genetic testing for APOE and other dementia-associated genes
By tailoring statin therapy to individual profiles, providers can enhance outcomes and support both heart and brain health. This approach is increasingly recommended by experts and major health organizations.
What Do Health Authorities and Experts Say?
Health authorities and experts emphasize the need for careful evaluation when prescribing statins to older adults. They acknowledge potential risks, including cognitive effects, and advocate for personalized treatment plans while monitoring patients' cognitive function during statin therapy.
Statements from the American Heart Association, NIH, and Alzheimer’s Association
According to recent statements from major health organizations, statins and dementia risk are closely linked through their effects on cardiovascular health. The American Heart Association emphasizes that managing cholesterol levels for a healthy heart indirectly helps protect against neurodegenerative diseases.
The NIH points to numerous observational studies suggesting that certain statins may offer a protective benefit against cognitive decline. However, the Alzheimer's Association notes that while there is ongoing research, a definitive causal link between statin use and a reduced incidence of Alzheimer's disease has yet to be established. They stress the need for further investigation to fully understand the underlying mechanisms.
Expert consensus on statin prescription for older adults
Recent studies show a more nuanced approach to prescribing statins for older adults. The goal is to balance the heart health benefits with any potential cognitive risks. Experts recommend carefully evaluating each patient's health profile. While statins are excellent for lowering cholesterol and reducing the risk of heart disease, their effects on thinking and memory can be different for each person.
This discussion highlights the importance of monitoring for cognitive issues and memory loss, especially in those who have a history of dementia or other similar diseases. Ultimately, creating a personalized strategy is essential for optimizing statin therapy for older people.
Clinical guidelines for monitoring cognitive function during statin treatment
Monitoring cognitive function during statin treatment is essential for older adults, particularly those with risk factors for dementia. Clinical guidelines emphasize regular assessments of cognitive abilities, especially for those on high-potency statins or with pre-existing conditions like high blood pressure or high cholesterol levels. Utilizing standardized cognitive tests can help identify potential declines in memory and overall function early. Additionally, healthcare providers should encourage discussions about statin therapy risks and benefits, enabling informed decision-making while considering individual patient health profiles and lifestyle changes that may mitigate the risk of cognitive impairment.
Conclusion
To summarize, understanding the relationship between statins and dementia means looking at the latest research and expert advice. Health authorities say that while statins lower cholesterol and reduce heart disease risk, concerns about cognitive side effects still exist.
It's important for doctors and patients to talk openly about the potential benefits and side effects of statin use. This is crucial for older adults who want to manage their heart health while also protecting their cognitive function as they age.
Frequently Asked Questions
Can discontinuing statins affect my risk of developing dementia?
It's not yet clear how stopping statin use affects the risk of dementia. Some studies suggest that stopping statin therapy could potentially speed up cognitive decline in people who are already at risk. You should always talk to your doctor for personalized advice on managing your statin use and cognitive health.
Are the cognitive side effects of statins permanent?
Research indicates that cognitive side effects from statins are generally not permanent. Most patients experience reversible symptoms upon discontinuation of the medication. However, individual responses may vary, necessitating ongoing monitoring and consultation with healthcare providers to address any concerns related to cognitive health.
What should I ask my doctor before starting or stopping statins?
Before you start or stop taking statins, have a detailed conversation with your doctor. Ask about potential side effects, how the medication might affect your memory and thinking, and if you need to be monitored for signs of dementia. Discuss lifestyle changes that can support your treatment, such as diet and exercise, and ask if there are any alternative medications. This will help you make an informed decision and ensure the best possible health outcomes.
References:
https://medlineplus.gov/ldlthebadcholesterol.html
https://nyulangone.org/conditions/dementia/types
https://www.alz.org/alzheimers-dementia/what-is-dementia/types-of-dementia/vascular-dementia
https://www.sutterhealth.org/ask-an-expert/answers/what-is-statin-therapy-1051061393
https://clarityxdna.com/blog/learn/what-is-a-cyp450-test-understanding-its-importance/
https://jnm.snmjournals.org/content/62/supplement_1/102
https://clarityxdna.com/blog/learn/pharmacogenetic-testing-unlocking-personalized-medicine/