Key Highlights
- Yeast infections, caused by candida albicans, are common and trigger symptoms such as vaginal itching, redness, and discharge.
- Over-the-counter (OTC) yeast infection creams and suppositories, such as Monistat and clotrimazole, are effective first-line options.
- Prescription medication, including oral Fluconazole (Diflucan) and Ibrexafungerp (Brexafemme), offers alternatives for stubborn or recurrent cases.
- Recognizing symptoms early can help you seek the right treatment and avoid complications.
- Consulting a healthcare provider is crucial for recurrent yeast infections or severe symptoms.
- Knowing the differences between OTC and prescription treatments empowers you to choose the best relief for your needs.
Introduction
Yeast infections are a common concern for many women, often causing discomfort and worry. These infections, usually driven by an overgrowth of candida albicans, lead to recognizable symptoms such as itching, irritation, and unusual vaginal discharge. If you’re noticing these signs, you’re not alone—most women will experience a yeast infection at some point. Quick and accurate treatment is key to relief, and understanding your options can help you take control of your health and restore comfort swiftly.
Understanding Yeast Infections
A yeast infection is a type of fungal infection that affects the vaginal area. It’s typically caused by a fungus called Candida, which naturally lives in the vagina in small amounts. However, when something upsets the natural balance of microorganisms, candida can multiply out of control, leading to a yeast infection, also known as vaginal candidiasis. This condition can be very uncomfortable and may return if not properly treated.
Understanding what causes a yeast infection is key to both treating and preventing it. So, what exactly triggers this overgrowth, and could some medications help stop it from returning?
Common Causes and Risk Factors
Hormonal shifts, antibiotic use, and a weakened immune system are a few reasons yeast infections can occur. For example, during pregnancy or certain phases of your menstrual cycle, your body’s chemistry changes. This can create an environment that allows the candida fungus to grow more easily. Additionally, when you take antibiotics for an infection, the medicine can kill off both helpful bacteria in your body and harmful ones. This imbalance causes yeast to multiply, which can lead to an infection.
Other risk factors include:
- Chronic illnesses that impact immunity, such as HIV or diabetes
- Wearing damp clothing or tight pants, which trap moisture near the vaginal area
- Use of certain feminine hygiene products with fragrances or dyes
- High-sugar diets, which feed yeast growth
Taking specific medications can help prevent yeast infections from recurring. This is especially true for people who experience them frequently. For instance, a doctor might prescribe an antifungal pill to be taken over several months. If you deal with frequent infections, a healthcare provider can work with you to create a personalized prevention plan.
Recognizing Symptoms That Require Treatment
Spotting the symptoms of a yeast infection early can make a big difference in your comfort. The most common indicators include relentless vaginal itching and burning that does not improve on its own. You might also notice thick, odorless, white vaginal discharge—often described as cottage cheese-like. Other signs include soreness, irritation, and redness around the opening of the vagina and vulva.
Look out for these symptoms:
- Intense itching in the vaginal area
- Vaginal discharge that is thick, white, and clumpy
- Redness and swelling of the vulva
- Soreness or burning sensations, especially during urination or sex
If you’re experiencing severe discomfort, recurring symptoms, or unusual discharge, it’s important to see a doctor. These symptoms can sometimes be signs of other conditions, such as bacterial vaginosis or sexually transmitted infections (STIs), so getting a proper diagnosis is essential.
Over-the-Counter Yeast Infection Medicines
OTC yeast infection creams, suppositories, and tablets provide convenient relief for mild to moderate symptoms. You’ll find a selection of vaginal creams and ovules at your local pharmacy, many of which offer single-dose or multi-day regimens. These products are designed for direct application to the affected area and often bring rapid improvement.
Choosing the right remedy is important, especially since home remedies lack strong scientific support. So, what are the most effective over-the-counter medicines for treating a yeast infection? Let’s explore the top options.
Most Effective OTC Creams and Suppositories
For over-the-counter treatment, products containing ingredients such as miconazole and clotrimazole are popular and effective choices. These antifungal medications are available as vaginal creams or suppositories and work by directly targeting the yeast causing the infection.
Creams are often sold with an applicator for simple use and are designed for treatment courses lasting one, three, or seven days, depending on their strength. Suppositories, sometimes called “ovules”, dissolve inside the vagina and can be a less messy alternative to creams. Many people find these options convenient and appreciate the quick relief they can offer.
Some key benefits include:
- Quick reduction in vaginal itching and irritation
- Simple, at-home use with clear instructions
- Several strength and duration options to suit different needs
Always read the directions carefully and complete the entire course for the best results. If your symptoms don’t improve, it’s time to consult a healthcare provider.
How OTC Pills Compare in Effectiveness
While over-the-counter options primarily consist of creams and suppositories, oral antifungal tablets are also available but require a prescription in the U.S. Knowing the difference between these treatments can help you have a more informed discussion with your doctor if you’re considering a prescription.
Prescription medications, such as Fluconazole. They are often a convenient choice, as a single pill can typically resolve most symptoms within three days. However, some people may require a longer course of treatment. Over-the-counter (OTC) topical treatments, on the other hand, are also very effective and have very few side effects that affect the entire body. For most mild yeast infections, both methods work well. The best choice for you may depend on what you find most comfortable and what your doctor recommends.
Prescription Medications for Yeast Infections
When over-the-counter options aren’t sufficient, prescription medications become important for treating severe or ongoing yeast infections. Oral medications, such as fluconazole and Ibrexafungerp, are approved by the FDA and work by targeting candida yeast cells throughout the body. For more stubborn cases, topical prescription creams containing ingredients like butoconazole or terconazole can also be used.
Understanding how prescription drugs compare to OTC choices can help you determine the best route for your situation. Next, let’s break down the types of prescription treatments available.
Types of Prescription Treatments (Oral and Topical)
Prescription treatments for yeast infections come in both oral and topical forms. Oral antifungal medications, such as fluconazole, are frequently recommended, particularly for severe or recurring infections. A single dose of these tablets can be very effective against the candida fungus, quickly easing symptoms such as vaginal itching and discharge.
Topical treatments, such as vaginal creams or suppositories, provide localized relief directly to the affected area and often contain antifungal agents like clotrimazole. Both the oral and topical treatments can help restore a healthy balance of microorganisms.
Effectiveness, Side Effects, and Safety Considerations
Prescription medications for yeast infections are highly effective, with cure rates above 90%. Oral antifungals such as Fluconazole and Ibrexafungerp circulate throughout the body, allowing them to tackle the infection from within. However, side effects can occur.
Common side effects include:
- Mild stomach upset and headaches
- Occasional nausea or diarrhea
- Rare allergic reactions, such as rash or swelling
Topical medications can cause localized burning or irritation. The FDA advises caution with oral antifungals during pregnancy, recommending topical therapy instead. If you experience severe symptoms or have a weakened immune system, prescription treatments may provide faster, more comprehensive relief. Always follow your healthcare provider’s advice to avoid complications and ensure the right treatment for your specific health profile.
Choosing the Right Yeast Infection Medicine for You
Picking the right treatment for a yeast infection depends on your symptoms, overall health, and past experiences with similar issues. Some women may find complete relief with OTC remedies, while others require prescription interventions for persistent or recurrent cases. Consulting a pharmacist or healthcare provider can help you evaluate your options and address any underlying concerns, especially if you have other health conditions that might impact your treatment choice.
Factors to Consider Based on Symptoms and Health Needs
Selecting the right treatment requires an honest assessment of your symptoms and circumstances. Here are a few considerations:
- If you have a weakened immune system (such as with HIV), prescription medication may be safer and more effective.
- Women with recurrent vulvovaginal candidiasis may benefit from long-term antifungal medication to prevent frequent episodes.
- Consider your menstrual cycle; some treatments may be less convenient during your period.
- If you’re pregnant, only use treatments recommended by a healthcare provider (typically a 7-day topical cream).
- Note any allergies or sensitivities to medication ingredients.
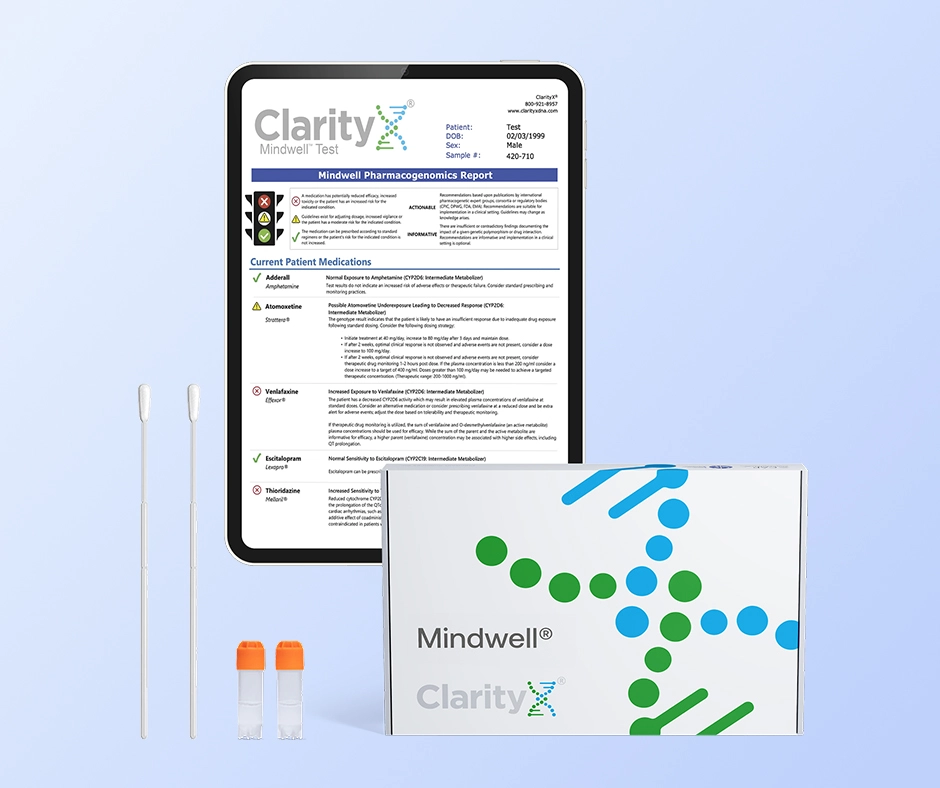
Personalizing Treatment with Pharmacogenetic (PGx) Testing
For women who experience recurrent or treatment-resistant yeast infections, the reason for treatment failure may lie in their unique genetic makeup. Pharmacogenetic (PGx) testing offers a data-driven approach to understand this issue. This type of DNA test analyzes key genes, particularly those in the CYP450 family, which instruct your body on how to metabolize common oral antifungal medications like fluconazole.
For example, a genetic test for medication might reveal that you are an "ultrarapid metabolizer" of a specific drug, meaning your body clears the medication too quickly for a standard dose to be effective. This can lead to persistent infections that seem unresponsive to treatment. Armed with this genetic insight, your healthcare provider can make a more informed decision, potentially by adjusting the dosage or choosing an alternative medication that better suits your genetic profile, finally breaking the cycle of recurrence
Choosing the right option often comes down to the severity and frequency of your symptoms. If you’re unsure, don’t hesitate to consult a healthcare professional for individualized advice. They can help tailor your treatment plan and address recurrent or complicated cases.
When to Seek Medical Advice Instead of Self-Treatment
While many yeast infections respond well to self-treatment, certain situations require professional evaluation. Reach out to a healthcare provider if:
- Your symptoms are severe, such as intense pain, swelling, or fever
- You have four or more yeast infections in a year (recurrent yeast infections)
- OTC medications do not bring relief after a full course
- You’re unsure if your symptoms are from a yeast infection or another condition
- You are pregnant or have a compromised immune system
Your provider can confirm the diagnosis, rule out more serious issues, and prescribe the right medication or further tests if needed. Ignoring persistent or severe symptoms can prolong discomfort and lead to complications, so it’s always better to play it safe.
Conclusion
To effectively manage a yeast infection, it’s helpful to understand the various treatments available and how they work. You have options ranging from over-the-counter creams and suppositories to prescription medication, so it’s important to know what might be best for your specific symptoms.
When choosing a treatment, consider potential side effects and your overall health. Remember, if your symptoms don’t go away or if they get worse. It’s crucial to get medical advice. Your comfort and health are the top priorities, so don’t hesitate to contact a healthcare provider for personalized guidance and to find the right path to relief.
Frequently Asked Questions
Can I use yeast infection medicine if I am pregnant or breastfeeding?
If you are pregnant or breastfeeding, it’s crucial to speak with your healthcare provider before using any medication for a yeast infection. While topical treatments, such as 7-day vaginal creams, are typically considered safe during pregnancy, oral medications are usually not recommended. Always follow professional medical advice to ensure your safety and the health of the baby.
How quickly do yeast infection medicines start working?
Most yeast infection medications, including antifungal creams and single-dose pills, start to relieve symptoms within 24 to 72 hours. Topical treatments can offer relief in just a couple of days, and oral medications like fluconazole often show improvement within three days. However, it can take up to a week for symptoms to fully clear up.
Is it safe to use yeast infection medicines with other medications?
Yeast infection medications are generally safe to use with most other drugs, but interactions can occur, particularly with oral antifungal medications. To avoid potential side effects or reduced effectiveness, it is important to inform your pharmacist or healthcare provider about all the medications and supplements you are currently taking.
References:
https://my.clevelandclinic.org/health/diseases/22961-candida-albicans
https://www.mayoclinic.org/diseases-conditions/bacterial-vaginosis/symptoms-causes/syc-20352279
https://www.hudipharma.com/2022/02/21/vaginal-ovule-and-suppository-for-women-well-being/
https://www.cdc.gov/std/treatment-guidelines/candidiasis.htm
https://clarityxdna.com/products/max-rx
https://clarityxdna.com/blog/learn/pharmacogenetic-testing-unlocking-personalized-medicine/
https://clarityxdna.com/blog/learn/what-is-a-cyp450-test-understanding-its-importance/