Key Highlights
- Reduces Trial and Error: Genetic testing for antidepressants provides data on how your body likely processes specific medications, helping to reduce the frustrating trial-and-error process with antidepressants.
- Focuses on Key Metabolic Genes: This mental health DNA test mainly analyzes genes from the Cytochrome P450 family, making CYP2D6 and CYP2C19 testing highly beneficial for assessing how you process over 80% of common antidepressants.
- Provides Actionable Clinical Guidance: Results classify psychiatric medications to assist clinicians in avoiding drugs that may be ineffective or cause side effects, enabling true personalized medicine for depression.
- Improves Patient Outcomes: Studies show that genetically guided prescribing can lead to faster symptom remission for conditions like Depression and Anxiety.
- A Tool for Collaboration: Pharmacogenetic testing for mental health is a supplementary tool, not a replacement for clinical expertise; it is most effective when combined with a thorough patient history and professional judgment.
Introduction
Every year, millions of people turn to antidepressants hoping for relief from Depression or Anxiety. Yet, the path to finding the right medication can be time-consuming and fraught with frustration. Many patients face a difficult cycle of antidepressant trial and error, juggling side effects, and wondering what to do when antidepressants stop working.
A DNA test for psychiatric medication uses a patient's genetic information to guide the selection of antidepressants and other psychiatric medications. Instead of relying solely on clinical experience, professionals can now match drugs to patients based, in part, on their unique DNA.
The Foundations: How Genes Affect Medication
Our bodies process medications differently. What works for one person might be ineffective or cause severe side effects in another. Some of this variability can be linked to genetic differences in how drugs are broken down. These principles of genetic testing for medication sensitivity apply to many psychiatric drugs used to treat various conditions, including ADHD, Bipolar Disorder, and PTSD.
Key genetic factors include:
- Metabolic Enzymes: Particular attention is paid to the Cytochrome P450 (CYP450) family, especially CYP2D6 and CYP2C19. CYP2D6 and CYP2C19 testing is crucial because variants in these genes can cause someone to process medication too quickly ("ultra-rapid metabolizer") or too slowly ("poor metabolizer").
- Transport Proteins: Genes like ABCB1 affect how drugs cross the blood-brain barrier.
- Receptor Differences: Variants in genes like SLC6A4 can influence how well a person responds to SSRIs.
To illustrate, consider how different CYP2D6 genotypes can affect medication levels:
SSRIs and SNRIs: A Closer Look at Antidepressants
Selective Serotonin Reuptake Inhibitors (SSRIs) and Serotonin-Norepinephrine Reuptake Inhibitors (SNRIs) are the most commonly prescribed classes of antidepressants. Their effectiveness and side effect profiles are highly influenced by the metabolic genes discussed above, making them a primary focus of pharmacogenetic testing.
SSRIs: This class of drugs works by increasing levels of serotonin in the brain. Common examples include sertraline (Zoloft), escitalopram (Lexapro), and citalopram (Celexa).
The CYP2C19 gene plays a crucial role in metabolizing both Lexapro and Celexa. A genetic test may reveal that a patient is a "poor metabolizer" via this pathway, putting them at a higher risk for side effects such as drowsiness or heart rhythm issues from a standard dose. With this knowledge, a clinician might instead choose a medication like Zoloft, which is less dependent on this single enzyme.
Atypical Antidepressants: Genetic testing also offers important insights for other classes, such as bupropion (Wellbutrin). Although primarily metabolized by a different enzyme, CYP2B6, its active metabolite is processed by CYP2D6. This means a person's CYP2D6 status can still significantly influence the drug's overall effect and side effect profile.
The CYP2D6 enzyme heavily influences the metabolism of these drugs. A patient identified as a "poor metabolizer" of CYP2D6 may experience significantly elevated levels of Effexor, thereby increasing the risk of side effects. On the other hand, an "ultra-rapid metabolizer" might clear the drug too quickly for it to be effective at a standard dose, requiring a dosage adjustment or an alternative medication.
SNRIs: These medications increase the levels of both serotonin and norepinephrine. Examples include venlafaxine (Effexor XR) and duloxetine (Cymbalta).
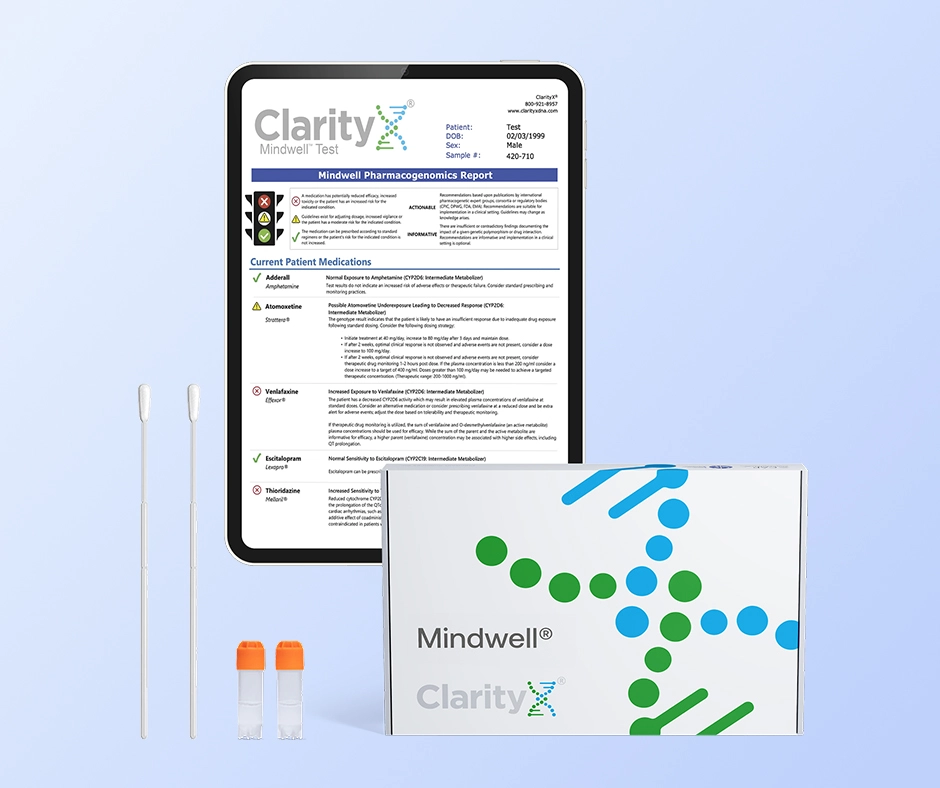
How Genetic Testing for Antidepressants Works
If you're asking, "how does genetic testing for antidepressants work?", the process is simple and non-invasive, typically requiring only a cheek swab or saliva sample. Laboratories analyze the DNA for specific variants to produce a report that answers the question, "what does a pharmacogenetic test tell you" about your likely interactions with many commonly prescribed medications.
Usually, these reports sort antidepressants into intuitive categories:
- Use as Directed: The patient’s genetic profile suggests a normal response.
- Use with Caution: A gene-drug interaction is possible; dose adjustments may be needed.
- Consider Alternative: A significant gene-drug interaction is likely, increasing the risk of side effects or treatment failure.
Nuances and Limitations
While compelling, it's crucial to understand the bounds of a mental health DNA test. The complexity of depression means no single test can "pick the perfect pill." Providers must integrate results with clinical judgment, using resources like the CPIC guidelines for antidepressants to apply findings within a comprehensive care plan that considers:
- Previous medication responses
- Co-existing medical conditions
- Patient preferences and lifestyle
- Other current medications
Genetic testing is an additional tool, not a substitute for expert clinical practice.
Real-World Evidence: What the Research Shows
Several trials have shown that integrating genetic guidance results in quicker symptom relief. The large-scale GUIDED trial, for example, demonstrated that patients whose treatment was guided by genetic testing were more likely to reach remission after eight weeks compared to those receiving standard care. Although the differences were often modest, they confirm that genetic data can significantly enhance the treatment process for psychiatric medications.
Insurance Coverage and Access
As with many medical innovations, insurance coverage for pharmacogenetic testing for mental health varies. Some plans cover it, particularly after a patient has failed to respond to multiple antidepressants. Others may not, and out-of-pocket costs can range from $300 to $2,000.
The Patient Experience: Stories from the Clinic
Clinical reports highlight the relief that data-driven guidance can provide. Patients asking "what to do when antidepressants stop working" often feel validated when a genetic test offers a biological explanation for their struggles. For example, a patient who learns they are a "poor metabolizer" of several SSRIs can work with their doctor to switch to a medication better suited to their profile, resulting in greater efficacy and fewer side effects.
Conclusion
The integration of genetic testing for antidepressants marks a pivotal shift toward personalized medicine for depression. While not a magic bullet, pharmacogenomic testing for depression provides an evidence-based tool that empowers clinicians and patients alike. By offering a glimpse into an individual's unique biology, it helps reduce the painful trial-and-error process and minimizes the risk of side effects. This data-driven approach represents a significant step toward ensuring individuals spend less time searching for a solution and more time truly feeling better.
Frequently Asked Questions
Will a genetic test identify the one perfect antidepressant for me?
A DNA test for psychiatric medication cannot pick a "perfect" pill. It identifies which medications are a better or worse match for your body's metabolism. This information helps your doctor make a more educated choice and avoid drugs that are likely to cause side effects.
My first antidepressant didn't work. Should I ask for a genetic test?
This is a great topic to talk about with your doctor. A mental health DNA test is especially helpful for patients who haven't responded well to at least one medication or have had significant side effects.
What does a pharmacogenetic test tell you?
A pharmacogenetic test shows how your unique genes may affect your response to certain medications. It detects variants in important genes that influence how your body processes drugs, which can help predict your chances of experiencing side effects or having a positive response to a specific drug and dosage.
How do I get a DNA test for psychiatric medication?
If you want to know how to get a DNA test for psychiatric medication, the first step is to schedule a consultation with your healthcare provider. They can assess your situation, determine if the test is appropriate for you, and order it from a certified lab.
Is this testing covered by insurance?
Coverage for pharmacogenetic testing for mental health varies widely. Some insurance plans cover it, especially after failed medication trials, while others may not. It is essential to check with your insurance provider about your specific policy and potential out-of-pocket costs.
References:
https://pubmed.ncbi.nlm.nih.gov/37788890/
https://pmc.ncbi.nlm.nih.gov/articles/PMC7692531/
https://files.cpicpgx.org/data/guideline/publication/serotonin_reuptake_inhibitor_antidepressants/2023/37032427.pdf
https://pubmed.ncbi.nlm.nih.gov/31721487/
https://clarityxdna.com/blog/learn/what-is-a-cyp450-test-understanding-its-importance/
https://clarityxdna.com/blog/learn/cyp2c19-the-gene-drug-metabolism/
https://clarityxdna.com/blog/learn/cyp2d6-gene-plays-major-role-drug-metabolism/
https://clarityxdna.com/blog/what-to-do-when-antidepressants-dont-work/